Women should get screened for breast cancer every two years beginning at age 40, according to draft recommendations under review by the U.S. Preventive Services Task Force.
The task force creates recommendations about preventive services for primary care providers. It last updated breast cancer recommendations in 2016.
Those recommendations, which are still active, suggest women ages 50 to 74 get screened every two years. Women ages 40 to 49 can decide individually whether to get screened, the guidelines say.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
That diverts a bit from the general guidelines offered by the American Cancer Society, which recommends women get mammograms every year starting at age 45 to find breast cancer early.
But there is some consistency among those health organizations that screening cisgender women or all those assigned female at birth in their 40s at least every other year offers the best chance to catch cancer early.
The mixed recommendations are confusing, acknowledged Dr. Mai Elezaby, associate professor and breast imaging section chief at the University of Wisconsin-Madison School of Medicine and Public Health and medical director of breast imaging at UW Health, during a recent appearance on “The Larry Meiller Show.”
Breast cancer is the second most common cancer in women, and 1 out of every 8 women is at risk of being diagnosed with it, according to the task force.
The draft recommendations come out of research that shows 19 percent more lives could be saved by screening all women beginning at 40 instead of at 50.
But there are many factors that play into whether a woman develops breast cancer, and conversations about the disease should begin with doctors as early as age 25, the National Institutes of Health says.
Elezaby explained that together, a patient and doctor can look at family history to determine whether the patient has a “higher than average risk” for developing the cancer. Then, they can make plans to start screening earlier.
Elezaby said some people are predisposed to getting breast cancer because of inherited genetic mutations. But, she said up to 70 percent of women who get breast cancer don’t have a recognizable risk factor.
“It is unfortunately a risk of just being a female,” she said.
Some patients may find new testing technology less painful
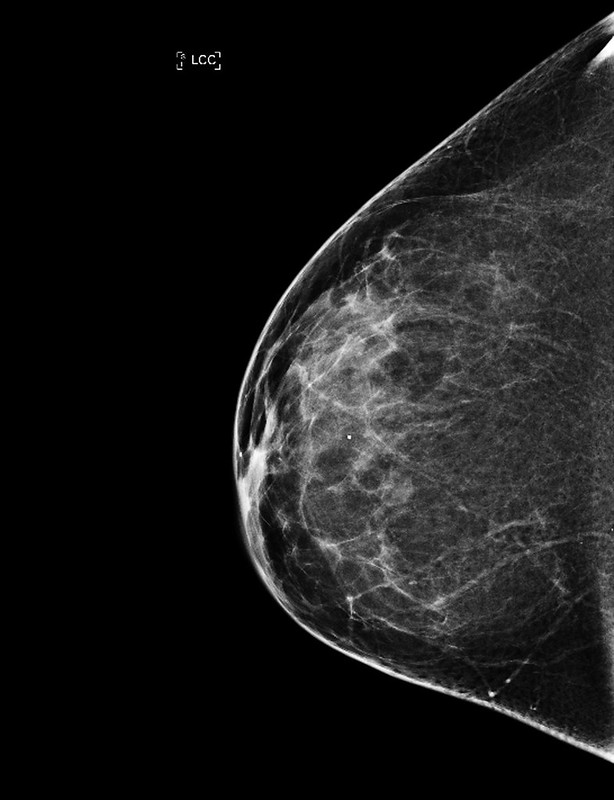
Mammography is the go-to test for seeking and identifying tumors in the breast.
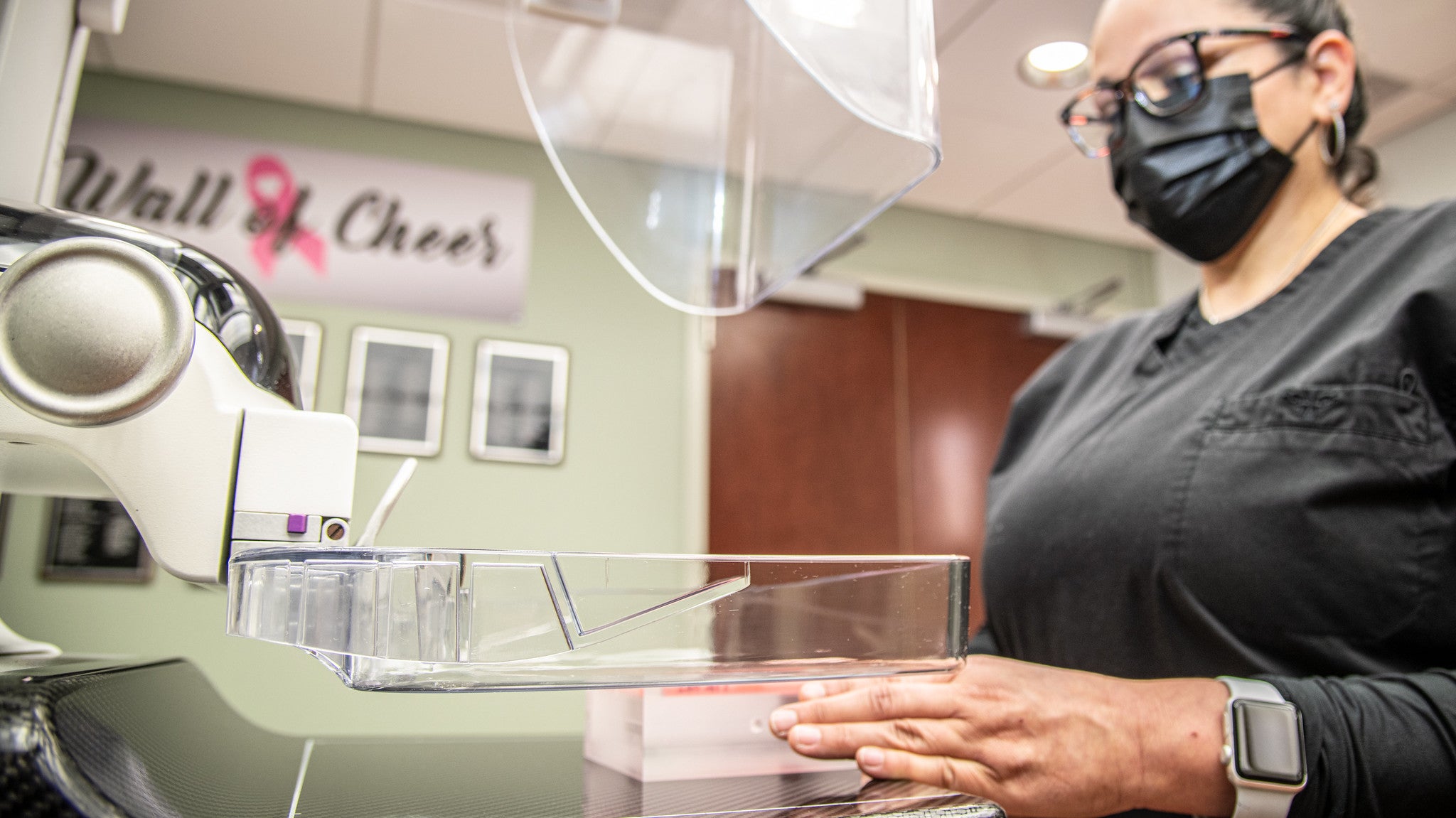
The device used to image the breast tissue has seen some updates in recent years, and many facilities are using that new technology called digital breast tomosynthesis, also called 3D imaging. Elezaby said the technology allows radiologists to see through the breast tissue and help find cancers early.
Better imaging also means fewer or no return visits for patients whose doctors may have previously needed to call the patient back to capture different views from imaging.
And, there’s the added benefit of it being less painful.
“Definitely the equipment itself, the way it’s positioned and how the breast is compressed, has improved to allow for less discomfort from the procedure itself,” Elezaby said.
While traditional mammography is typically covered by all insurance companies with no out-of-pocket expenses, not all cover tomosynthesis. Medicare, for one, does cover tomosynthesis with no out-of-pocket expenses, Elezaby said.
It’s best to check ahead of time what technology your provider uses and what your insurance will cover.
A 2023 bill that would have required health insurance companies to cover additional breast cancer screenings and diagnostic exams never got a vote in the state Senate or Assembly.
Be aware of overall breast health
Elezaby said that in patients for whom cancer is detected early, there’s a 98 percent chance of survival.
Elezaby said “early” means a stage 0 or stage 1 cancer diagnosis, as opposed to stages 2 through 4. Staging is a complex analysis of the size of the cancer, whether it has spread, the type of tumor it is and whether it responds to certain hormones or receptors.
“Not all cancers are the same, and not all types of cancer are the same,” Elezaby said.
Although finding breast cancer early is an important part of successful treatment, the general recommendations for women now are more about being aware of overall breast health and much less about performing self exams.
“It’s really hard to be very vigilant about doing your self breast exam and be able to identify if there are changes or not,” Elezaby said. “But as long as you’re aware of changes that are happening in your breast, that you don’t see any skin changes or nipple changes, or if there are any changes that you notice to seek help and go in to see your health care provider, that’s what we are asking of our patients.”
The clinical breast exam should be performed by a trained health provider, Elezaby said. That professional knows what to expect and what may constitute a change for the patient.
Wisconsin Public Radio, © Copyright 2024, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.