Everyday movements like grabbing a cup of coffee or sending a text message start with signals in the brain. But when an injury or illness disrupts the connection between the brain’s neurons and other parts of the body, those actions can become seemingly impossible.
On Monday, as part of a week-long series about medical innovations and advice, Wisconsin Public Radio’s “The Morning Show” invited two doctors to discuss breakthroughs in brain-computer interfaces that aim to restore physical abilities.
Here are three takeaways from the program:
Stay informed on the latest news
Sign up for WPR’s email newsletter.
‘A new era’’ and who it helps
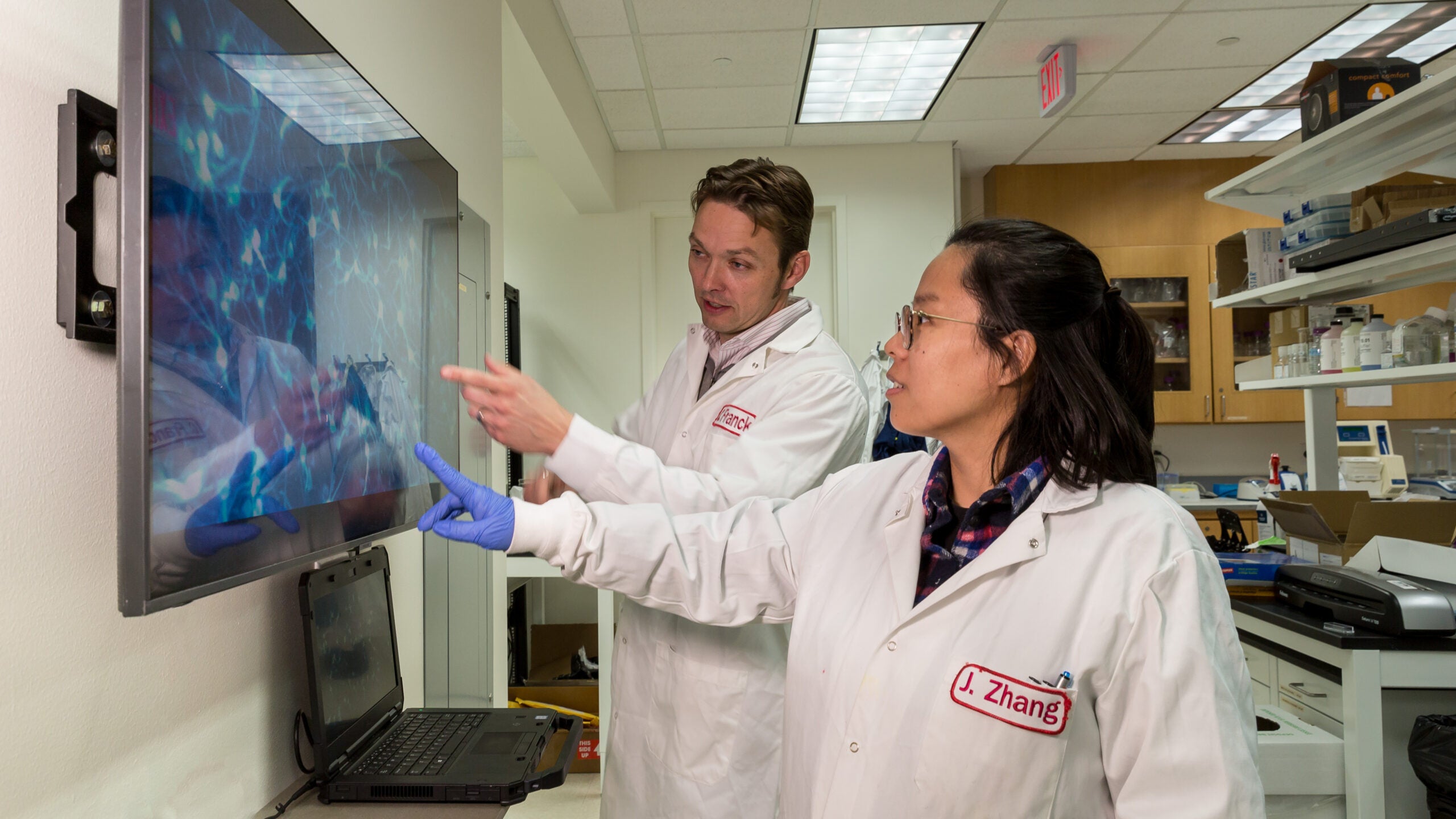
Dr. Leigh Hochberg is a neurologist who leads the Center for Neurotechnology and Neurorecovery at Massachusetts General Hospital and directs a research team that is developing technology for brain-computer interfaces. He said the devices can help people with spinal cord injuries that result in the inability to move one’s arms or legs, as well as people with ALS or a brainstem stroke.
The Centers for Disease Control and Prevention estimates an average of 5,000 new cases of ALS are diagnosed each year.
“I think the potential for this field is substantial,” Hochberg said.
Last summer, Dr. Shahram Majidi implanted a device on the brain of a patient with severe paralysis from ALS, the progressive nervous system disease also known as Lou Gehrig’s disease. The procedure to implant the device was the first of its kind in the nation.
Since then, the professor at the Icahn School of Medicine at Mount Sinai in Brooklyn said he has worked to implant devices in the brains of two other patients as part of the safety and feasibility stage of a clinical trial.
“We are very hopeful that this will be the beginning of a new era,” he said.
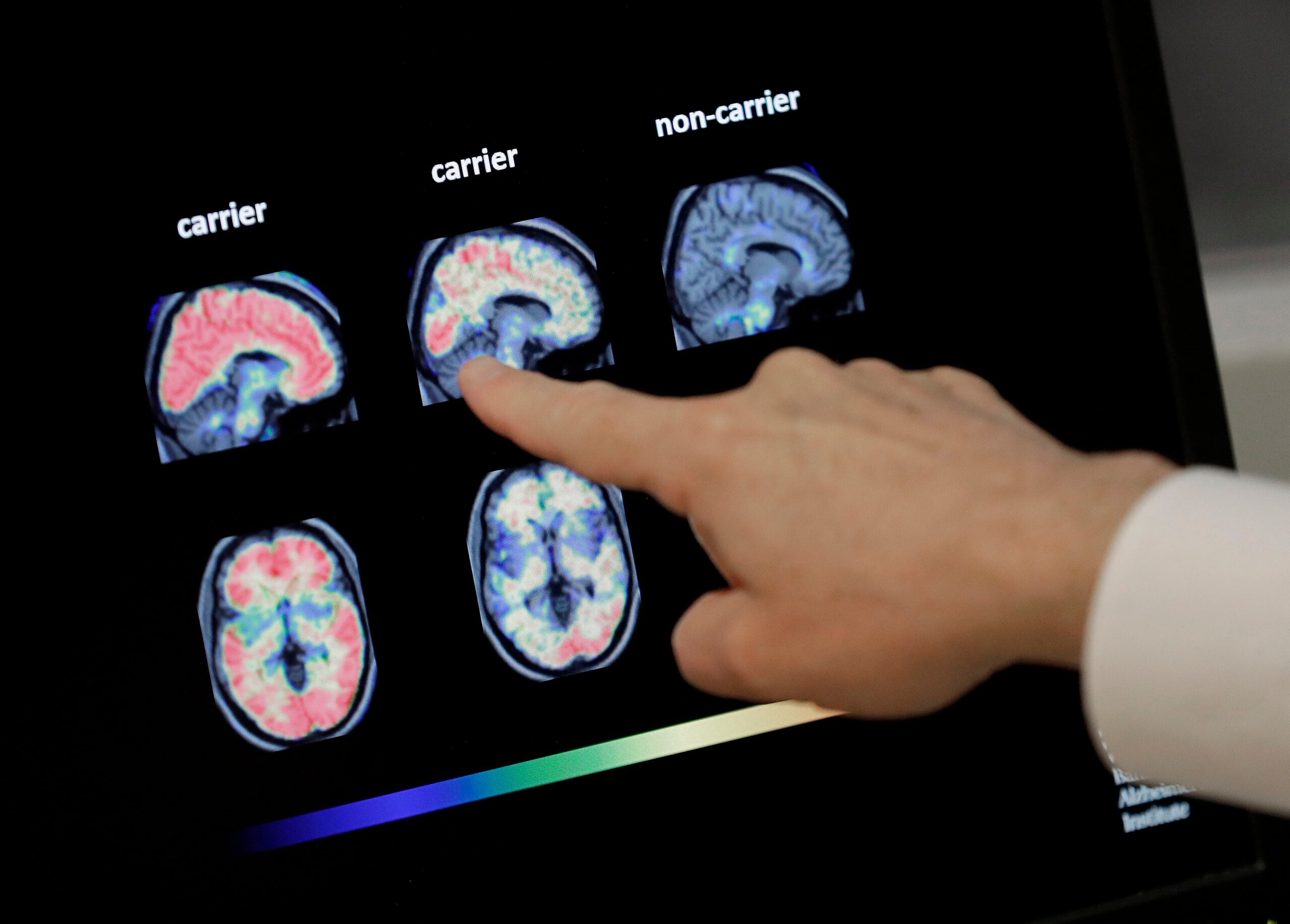
Brain-computer interface devices aim to allow performing some actions by thought alone, according to a Bloomberg report on the breakthrough patient. The devices translate brain activity into commands on a computer.
Majidi said after a few weeks of training, his patients can send a text message, shop online and notify a caregiver if they need help.
“I think that is a significant improvement in quality of life for someone who is bedridden and completely disconnected from the outside world,” he said.
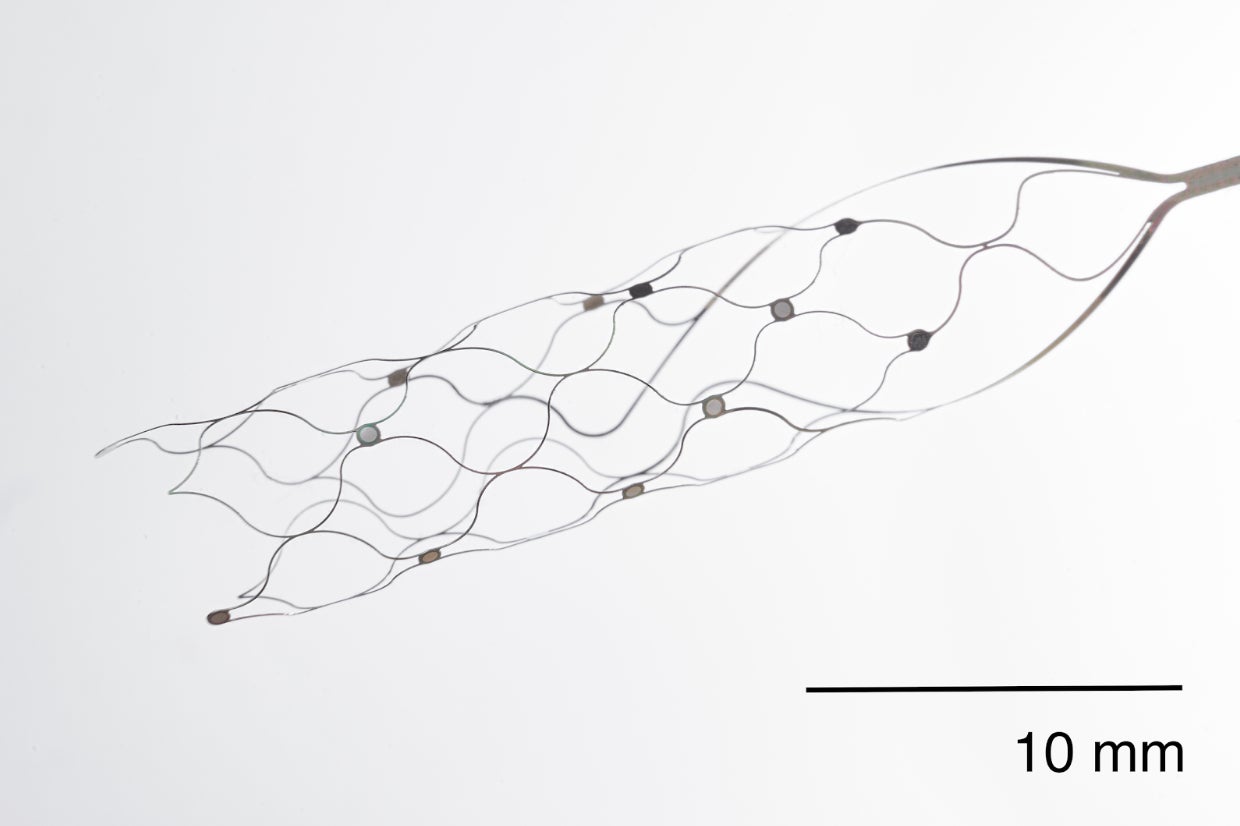
Making the procedure minimally invasive
Majidi said brain-computer interface devices previously required open-brain surgery by drilling a hole into the brain and implanting the device within the brain tissue or on the brain’s surface.
Now, he said, doctors can go through the “natural highway of the brain” — the veins. A tiny catheter goes through the vein until it reaches the brain and deploys the device.
The goal of these devices is to be invisible and fully implanted, similar to cardiac pacemakers or deep-brain stimulators for those with Parkinson’s disease, Hochberg said.
“There are millions of pacemakers, hundreds of thousands of deep-brain stimulators that have been placed,” he said. “To the observer of somebody who is using one of these devices, they’re essentially invisible because they’re fully implanted.”
Balancing risk, rewards and patience
Hochberg and Majidi acknowledged that a lot of research and work remains before brain-computer interfaces could become mainstream.
Early stage clinical studies are meant to carefully and rigorously look for adverse events that happen after device implantation, Hochberg said. Even rare adverse effects need to be part of the consideration for patients.
“The most important person making that decision is going to be the person themselves who is considering using that device,” Hochberg said.
Majidi commended multiple ongoing efforts by different companies to run their own clinical trials. While none of the devices so far have been perfect, the cumulative effort from everyone is going to help the sickest of patients, he said.
Majidi estimated more than 5 million people in the United States live with severe paralysis, including people who have suffered from a stroke, demyelinating disease, neurodegeneration such as ALS, or from trauma such as a car accident.
“These efforts eventually help us to identify some of these patients that we can help become a little more independent in their daily life — to communicate with the outside world and be able to enjoy doing their daily activities,” he said.
“Body Week” is a week-long series on Wisconsin Public Radio’s “The Morning Show.” An hour of the program is dedicated each day to one part or system of the body. Monday’s show featured the brain. Next, we explore the heart. Listen to the show weekdays at 8 a.m. on The Ideas Network. Submit your questions about the body to ideas@wpr.org.
Update: This story was updated Feb. 8 to add more context to Dr. Leigh Hochberg’s line of work.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.