As Wisconsin heads into a second winter battling COVID-19, new infections are as high as they were last December. A record number of patients are on ventilators and some hospitals are turning away ill and injured people who are then sent to facilities hundreds of miles away.
In a single day, 28 patients who recently sought care in Green Bay — including three people suffering strokes — had to get care elsewhere, said Dr. Ashok Rai, president and CEO of Prevea Health.
“One family had to go over 200 miles away just to get back care that they needed. This wouldn’t happen if we had the beds and the staff available,” Rai said during a briefing with state health officials Thursday where they said high case rates driven by the delta variant are straining hospital capacity.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
Statewide, 97 percent of intensive care beds are in use and in some parts of Wisconsin there are no beds available. Wisconsin Hospital Association data shows the Fox Valley had zero ICU beds and no intermediate beds as of Wednesday. In western Wisconsin, it was the same situation.
Still, state Department of Health Services Secretary-designee Karen Timberlake said an auxiliary, or field hospital like the one in West Allis that was set up early in the pandemic, isn’t necessary at this point.
“We have space for people. We need to make sure we had adequate staffing along the continuum of care,” she said, noting the state has contracted with agencies to provide additional health care workers in hospitals and has eased regulations so that certified nursing assistants can be trained more quickly to shore up staffing shortages in nursing homes.
The seven-day average number of COVID-19 cases in Wisconsin climbed to 3,015 on Thursday, as researchers around the world try to determine how fast the newest variant, omicron, spreads — and whether it causes more severe disease. Omicron has yet to be found in Wisconsin, but it has been detected in Minnesota, officials there confirmed on Thursday.
Nearly all the cases sequenced in Wisconsin are the delta strain, which Rai said is resulting in patients who are younger, sicker and need care longer.
More patients than ever are on ventilators, said Timberlake. On Nov. 30, 688 people with COVID-19 needed mechanical help to breathe. The previous high was 638 on Nov. 18, 2020.
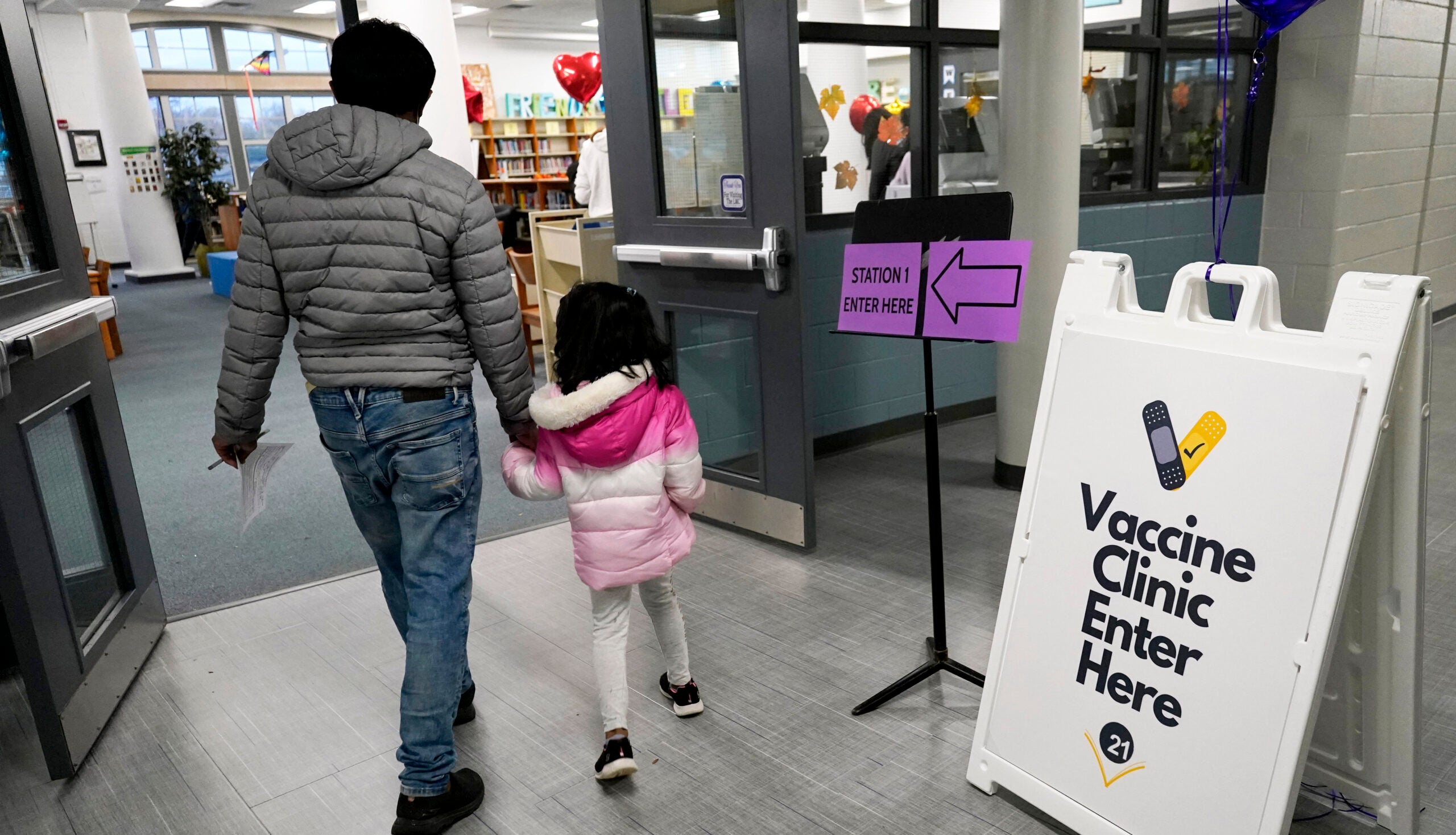
State health officials urged everyone 5 and older to get vaccinated against the disease and for adults to get booster shots, pointing to data that shows unvaccinated people are nine times more likely to be hospitalized for COVID-19 than those who have had their shots, and 11 times more likely to die compared to those who are vaccinated.
In Wisconsin, 56.1 percent of the eligible population has been fully vaccinated against COVID-19, DHS reports. And more than 87,000 children age 5-11 have received their first shot since early November, Timberlake said, when federal regulators approved Pfizer vaccine for that age group.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.