Everyone, and I mean everyone, should have an advance directive. Let me review what that is and why it’s so important.
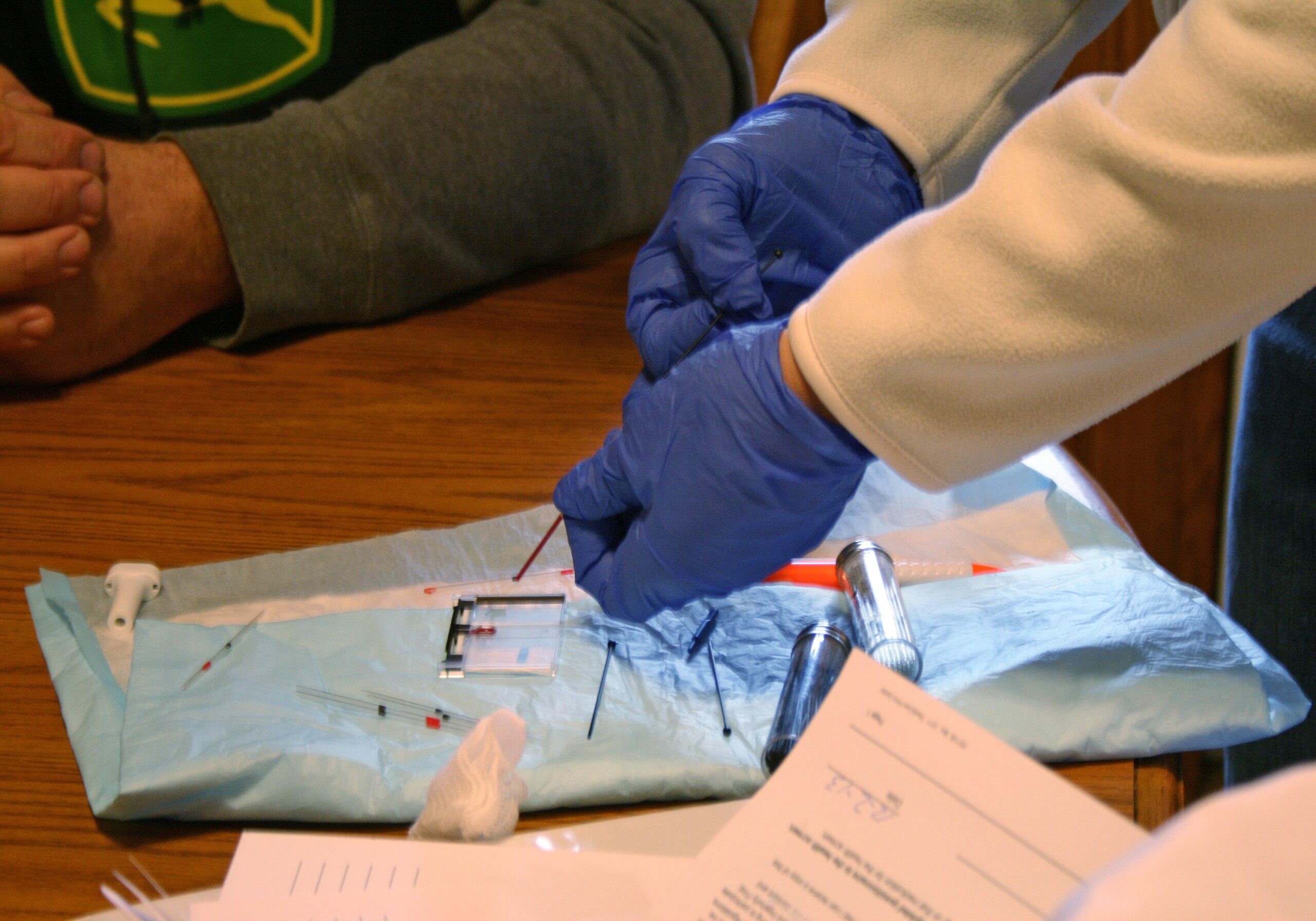
An advance directive, also called a durable power of attorney for health care, is a legal document that provides specific instructions for your medical care if you are unable to communicate for yourself.
This might seem like something only older folks need, but you never know when you’re going to die. You think you might have some idea, but you really don’t. As a doctor of 45 years, let me tell you: People think they’ll live forever — even the old ones, and I am one of those.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
At 77, I still ski and hike. I have some arthritis and a few other maladies, but I think I’ll live a long, long time. Yet, the numbers don’t say that. I have a 50 percent chance of a five-year life expectancy. If something happens to me and I don’t have an advance directive, then some judge somewhere might decide whether I go on a ventilator or not.
What about when you’re young? Even though death seems like a faraway afterthought, we all know someone who has ended up in the hospital suddenly from a fall or car accident, a cardiac arrhythmia or drowning.
There was the famous case of Terri Schiavo. For 15 years, she was kept alive in a persistent vegetative state because she never signed an advance directive allowing her husband to remove her feeding tube. She was 41.
I’m just trying to hit home that an advance directive is not something exclusively for old folks. Everyone should have one, just like everyone should have a will — and maybe an extra set of keys you hide under that potted plant in case you get locked out of the house. It’s good planning.
When you sign one of these, it outlines your health care wishes. But most importantly, it designates someone who can make the decisions for you. You can put down whether you want a temporary or permanent feeding tube, being put on a ventilator, stuff like that. But in the end, it’s the person you designate who makes sure that will happen.
This is only the first step of the process. The more important step is discussing it with the loved one or loved ones you choose to name in the document so they can make the decisions you want. The more you clarify this, the better it will be. Let me tell you, I have seen many families torn apart because they’re not on the same page.
Doctor and author Atul Gawande coined this problem as the “seagull effect.”
Picture this. You and your siblings have been taking care of mom for years. She’s now seriously ill, in the hospital, on a ventilator for a week. You’ve been doing the heavy lifting all these years with her health, with one sibling who lives out of town in California who has not taken as much of an interest. They fly in, and even though lots of thought has gone into the decision to pull the plug, they throw a wrench in the plan. An awful family argument then ensues.
The best way to prevent this is with a clear path — talking to your loved ones about what you want done or not done and designating one person to be the final person who makes the call. A well-planned advance directive plays a critical role here.
My spin: Everyone should have an advance directive, signed and dated. You can pull down a free form from the state of Wisconsin. Or you can pick up one at your doctor’s office. Then follow the directions, sign and date it, and bring it back into the doctor’s office so it can be entered into your medical record.
This column is the opinion of the author, © Copyright 2025. Dr. Zorba Paster is a family medicine physician practicing in southern Wisconsin. Consult a health care provider for personal health information. The opinions expressed aren’t meant to reflect the views of Wisconsin Public Radio, its employees, the University of Wisconsin-Madison or the Wisconsin Educational Communications Board.
Zorba Paster On Your Health airs on WPR News Saturdays at 1 p.m. and Sundays at 6 p.m.