People with diabetes often hear that they face higher risks of severe complications from COVID-19, the disease associated with the novel coronavirus. But why? And what precautions should they take?
Wisconsin Public Radio and Wisconsin Watch compiled your questions and sought answers from Dr. Dawn Davis. She is director of the Comprehensive Diabetes Center at the University of Wisconsin-Madison and section chief for Endocrinology at the William S. Middleton Memorial Veterans Hospital in Madison.
Davis offered her insight while cooped up in her “crazy-crowded house” — with her husband, three children, two cats, one dog, many fish and two European houseguests who “won’t be going home any time soon.”
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
This transcript has been edited for brevity and clarity.
Q: By far the most common question we heard: If I have diabetes, am I more susceptible to contracting the virus or more susceptible to worse outcomes? Or is it both?
Dr. Dawn Davis: Unfortunately there’s still a lot that we don’t know about this virus, because it’s so new, and there are not a lot of published, well-controlled studies about it yet.
Researchers in China who dealt with the outbreak published a paper suggesting an increased risk of the severity of outcomes in patients who had diabetes. They saw more hospitalization, ICU care and overall mortality in patients who had diabetes.
It’s hard to know if those patients were already in the hospital and more exposed to the virus, or if they would have had a higher risk of problems had they been living in the community and been exposed to the virus. There’s a lot we just don’t know.
But our advice to people with diabetes is, yes, they should consider themselves at higher risk of more severe outcomes if they contract the virus. Avoiding getting it is the goal.
Q: What makes someone with diabetes potentially more susceptible to a viral infection?
DD: Globally, we know diabetes patients are more susceptible to infections and tend to have more severe outcomes during other viral infections and outbreaks. That includes H1N1 influenza, and even seasonal influenza.
One big reason: There’s an impact on the immune system in patients who have diabetes. They may have increased baseline inflammation, and they also may be unable to mount a response to an infection as robustly as other patients.
In addition — especially with Type 2 diabetes — diabetes comes along with multiple other medical problems, including heart disease and high blood pressure. All of those things can contribute to poor outcomes if patients get an infection.
Q: Parents of children with diabetes asked us this question: Children are said to have a lower risk of developing a serious illness from coronavirus. Is that true even with children who have diabetes?
DD: We don’t know the answer to that question for this particular illness. Children certainly do seem to be somewhat more protected in the case of (COVID-19). That hasn’t been the case for other viral outbreaks. So there’s something a little bit unique about how this virus impacts children.
However, it’s not impossible for children to be infected or to have severe outcomes from coronavirus. It’s certainly not something to be blasé about.
And yes, Type 1 diabetes may slightly increase the risk of worse outcomes for infected children. It’s probably a lower risk than for an adult — certainly for an older adult.
Q: What precautions should people with diabetes be taking?
DD: They should follow all recommendations to minimize their social contacts. That includes trying to stay home and avoiding other public places and people as much as possible.
We here at University of Wisconsin-Health and the VA are working hard to minimize the number of patients coming into our facilities. We’re converting a lot of patients to telephone visits or virtual visits if we can. If you have a routine visit scheduled, contact your provider about rescheduling or holding it over the phone.
We want to make sure patients are still getting care. I don’t want people just canceling their appointments.
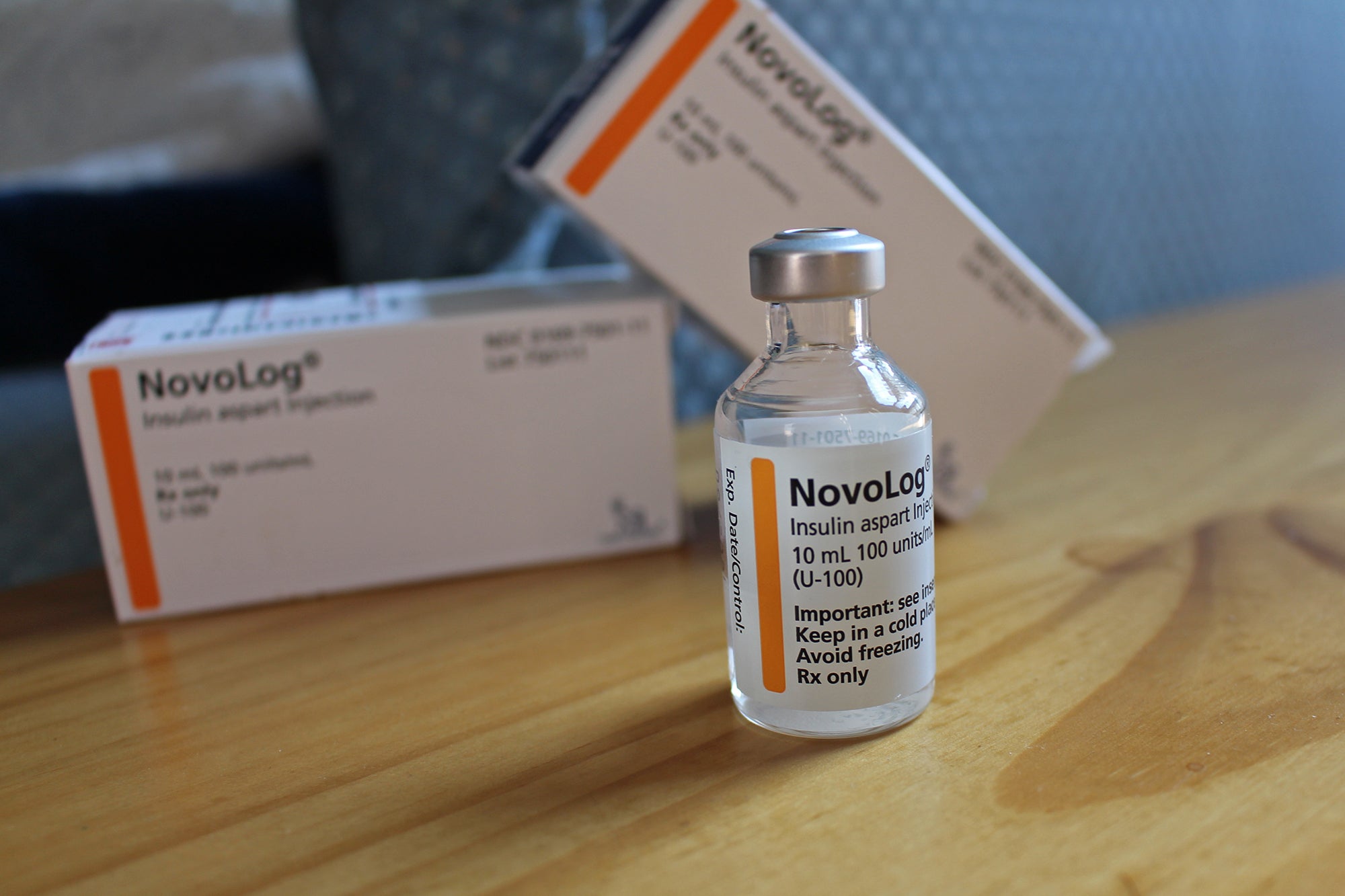
Q: Are there any supplies or medicines that people should stock up on?
DD: We don’t want to encourage people to advance-order tons of excess supplies. That could decrease the availability of supplies for people who need a standard refill or need to renew their supplies.
But now is a good time for patients to take stock of what they have in-house. They should have a 30- to 90-day supply.
Converting prescriptions to 90-day supplies is a good idea. It’s also a good idea to set up mail-order prescriptions — to avoid having to go to pharmacies, which may not remain open all the time.
Patients should also assess whether they have appropriate backup supplies. For example: We want our patients who use insulin pumps to have a backup supply of insulin if they needed injections.
We always have these guidelines for our patients, but now is a good time for everybody to make sure they’re thinking about those things and following up with their providers.
Q: People with diabetes say they are frustrated that they can’t get insurance companies to approve a 90-day supply of insulin. What should those patients do?
DD: That’s a real issue for a lot of people — not just with insulin, but with diabetic test strips and all kinds of things.
We don’t have any reason to anticipate a major shortage or supply chain issues. So I don’t know that we need to panic about not having a 90-day supply. If your insurance only allows the 30-day supply, you don’t have a ton of options — other than asking your insurer to waive their limit.
My advice is to continue to reach out to your providers if you are concerned.
That’s the other advantage of setting up mail-order prescriptions. By automating the process, you won’t have to worry about your local pharmacy running out of stock.
Q: For people with diabetes living in an area with community spread of coronavirus, is it safe to take your dog for a walk?
DD: I’m not an infectious disease expert, and I’m not part of the public health team. But from what I understand from current guidance: Yes, if you go outdoors that is perfectly fine.
Again, limit your contact with other people. So don’t go to a crowded dog park or talk to five different people at close range.
We encourage people to do that as much as possible, because we want people to get a little bit of exercise — get a little bit of activity and break up the boredom and depression of sitting in your house all day.
Q: What else do you want people to know?
DD: Patients who have diabetes — and particularly patients who have diabetes and other medical problems — need to be strict about social distancing and isolation to keep themselves safe.
That doesn’t mean that their medical providers don’t want to hear from them. We are all a bit overwhelmed with phone calls, and there might be some delays, but checking in and asking questions is the right way to go.
We’ll all get through this together.