The U.S. Department of Labor is suing a third-party health insurance administrator based in Wausau for wrongfully denying thousands of emergency room and urinary drug screening claims.
Federal officials say UMR Inc., a subsidiary of the Minnesota-based UnitedHealth Group, improperly denied insurance claims for more than 2,000 people since January 2015.
The labor department filed a lawsuit in federal court last Monday, after an investigation found the company’s process for evaluating emergency room claims allegedly did not comply with the law, relying solely on diagnosis codes and not the “prudent layperson” standard.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
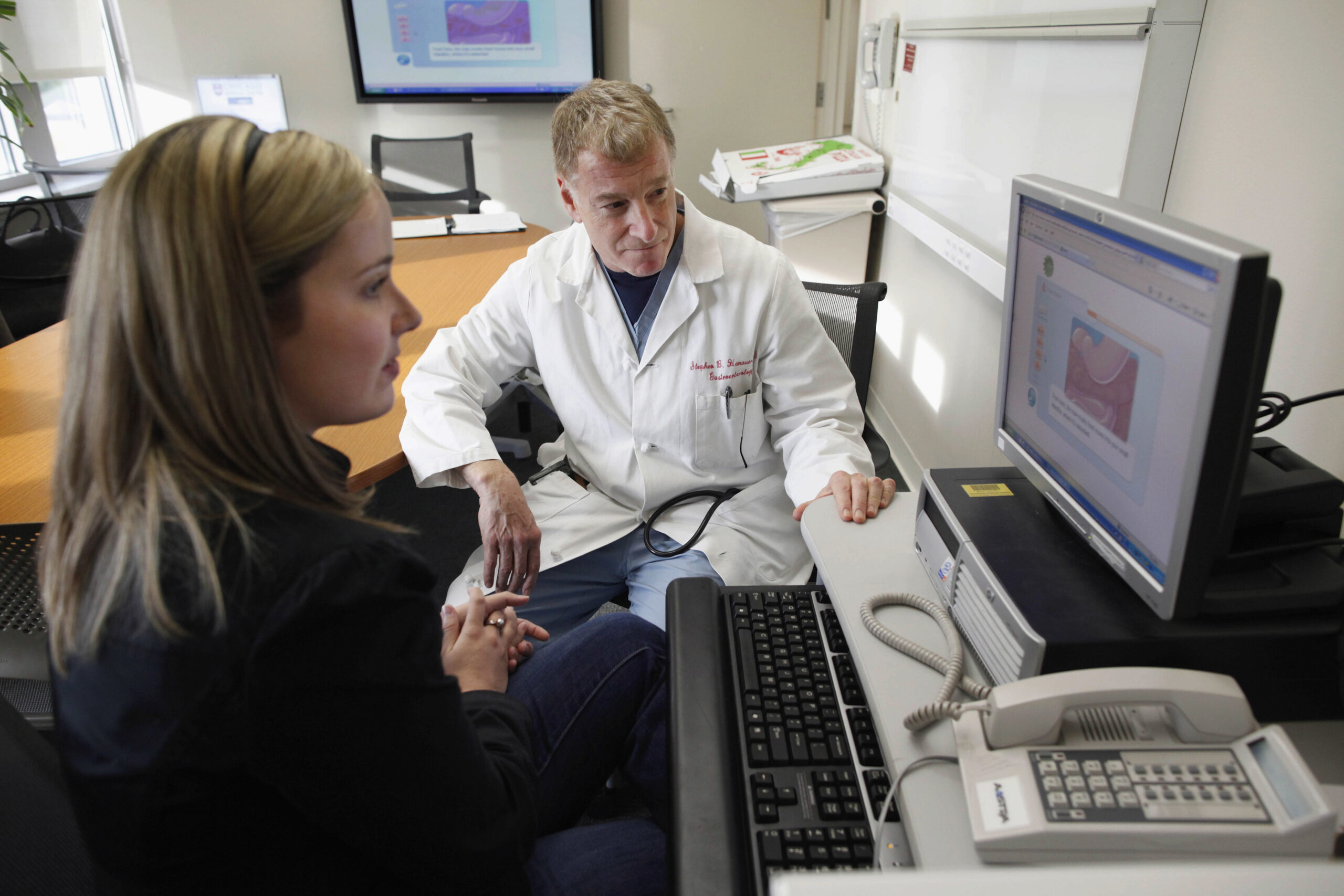
Ruben Chapa is regional director for the U.S. Department of Labor’s Employee Benefits Security Administration. He said the prudent layperson standard requires insurers to look at whether someone seeking emergency treatment believed they required immediate care.
“For example, you’d have an instance where an individual goes in with heartburn but doesn’t believe that it’s heartburn; he or she believes it’s a heart attack,” Chapa said. “If the individual really believed that it was a heart attack, then most insurance plans would cover that.”
UMR also allegedly denied nearly all urinary drug screening claims without reviewing them for medical necessity.
Chapa said drug screenings can be medically necessary for multiple reasons, ranging from ensuring a patient’s substance abuse treatment program is moving in the right direction to ensuring a medication doesn’t have a negative reaction with another substance in someone’s system.
He said UMR’s claim denials have had major health and financial consequences for those affected.
“There’s a significant impact to an individual’s health and welfare,” he said. “Individuals, in some instances, have gone bankrupt because there’s large expenses that are sometimes associated with the treatment they received.”
The lawsuit seeks reimbursement for those with wrongfully denied claims, and asks the court to prevent the company from continuing that practice.
In a statement, UMR said the lawsuit is based on an administrative process that’s no longer in place.
“We have been in ongoing conversations with the (Department of Labor) regarding this matter and will continue to defend our position vigorously,” the statement read.
Chapa said the department is interested in resolving the matter and ensuring individuals are reimbursed, but it still has to confirm the company’s claims that there’s a new process in place.
“While they’ve identified potential changes they might make, it was never clear that they’ve instituted those changes, and it’s not clear that the changes they’re making are sufficient to comply with the law,” he said. “That’s why this enforcement action is so important, because we want to make certain that a judge orders UMR to comply with the law.”
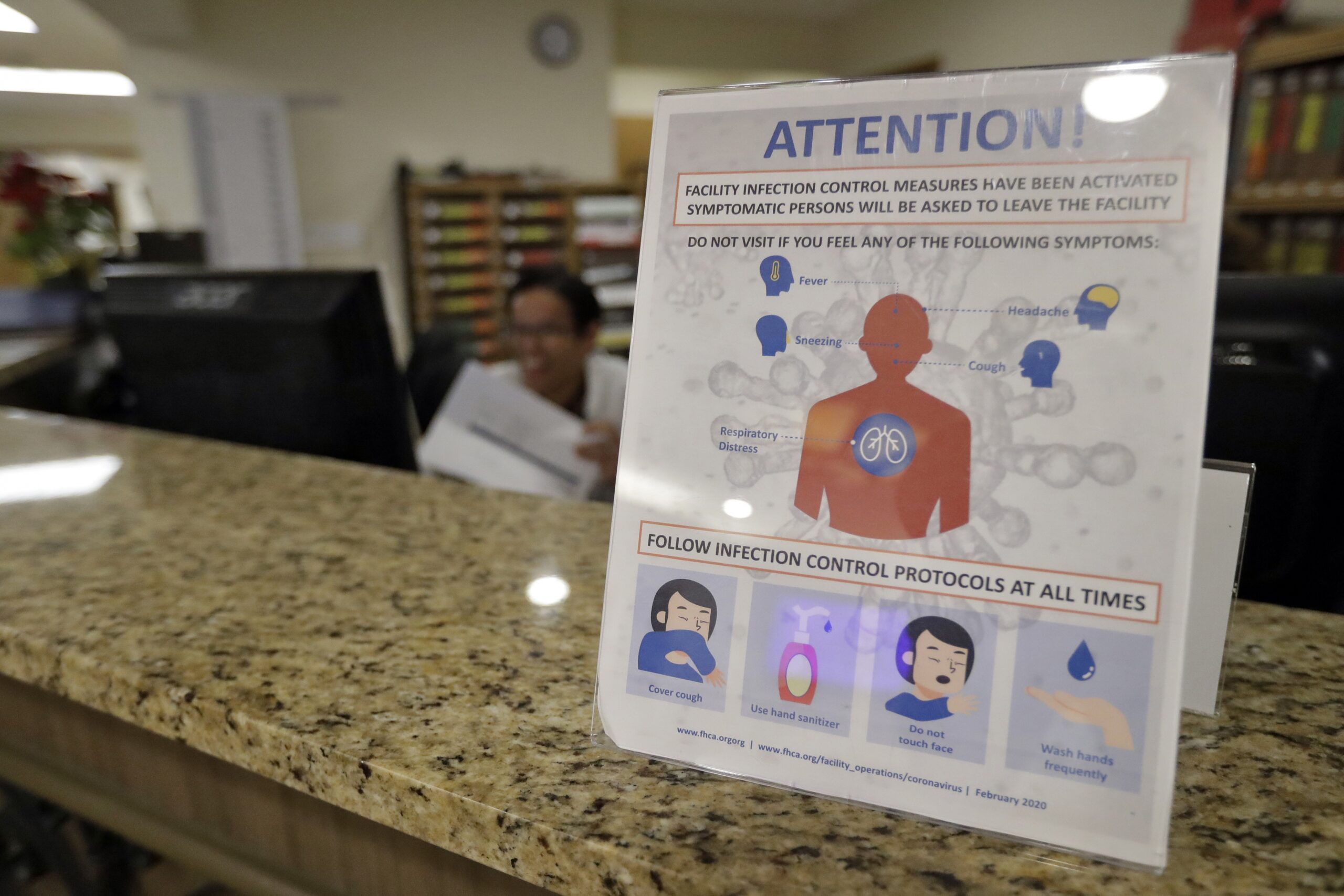
UMR’s parent company, UnitedHealth Group, faced criticism from health care providers in 2021 when it announced a plan to halt payments for “non-emergency” care in emergency rooms.
At the time, the American Hospital Association sent a letter to the insurer that said such a move would put patients’ health and wellbeing in jeopardy.
“Patients are not medical experts and should not be expected to self-diagnose during what they believe is a medical emergency,” wrote Richard Pollack, president of the American Hospital Association. “Threatening patients with a financial penalty for making the wrong decision could have a chilling effect on seeking emergency care.”
The Star Tribune reported that UnitedHealth Group’s plan to stop payments for non-emergency care in emergency rooms was halted.
The Department of Labor’s allegations may be part of a larger, industry-wide pattern. Dr. Christopher Kang, president of the American College of Emergency Physicians, said in a statement that large insurance companies do everything they can to deny, delay or reduce payments for emergency care.
“While emergency physicians are required to provide care when a patient needs it, insurance companies regularly violate rules that require them to cover the cost,” he said. “Immediate action to strengthen enforcement of the prudent layperson standard and other existing laws can help hold insurers responsible for their rampant bad behavior and protect patient access to emergency care.”
The Wisconsin Department of Health Services website provides information about what individuals can do if they feel their insurance claim was wrongfully denied.
Chapa added that individuals concerned about wrongfully-denied insurance claims can also contact the Department of Labor’s Employee Benefits Security Administration to connect with a benefits advisor.
“One of the really nice things about it is that you’re speaking to a live person,” he said. “These individuals are excellent at identifying the issues and helping plan participants work through any potential issues they have, and helping employers. They will contact the employer and try to work through any issues they have, so that it may prevent any of these enforcement actions.”
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.