Radiation-emitting drugs, or radiopharmaceuticals, are increasingly used to target and kill cancer cells with positive results for patients.
In July, during an appearance on Wisconsin Public Radio’s “The Morning Show,” the 2023 crowned Miss America Grace Stanke said her father’s cancer treatment with nuclear medicine had in part inspired her to study nuclear engineering.
“He is alive today because of nuclear medicine. It helped save his life, and I couldn’t be more thankful,” said Stanke, a Wausau native and student at the University of Wisconsin-Madison.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
While some radiopharmaceuticals have been utilized in thyroid cancer treatment for decades, new radiation drugs are showing promise in many other areas, according to Dr. Steve Cho, a professor and section chief of the nuclear medicine section of the Department of Radiology at the University of Wisconsin-Madison’s School of Medicine and Public Health.
Cho recently joined “The Morning Show” to discuss what’s exciting about new developments in nuclear medicine, shortages of nuclear material needed for treatment and the safety of treatments.
The following was lightly edited for brevity and clarity.
Kate Archer Kent: According to recently published data from the World Nuclear Association, over 20 million procedures using radiopharmaceuticals and imaging instruments are carried out each year in our country. Why has there been this explosion of research and clinical trials involving nuclear pharmaceuticals?
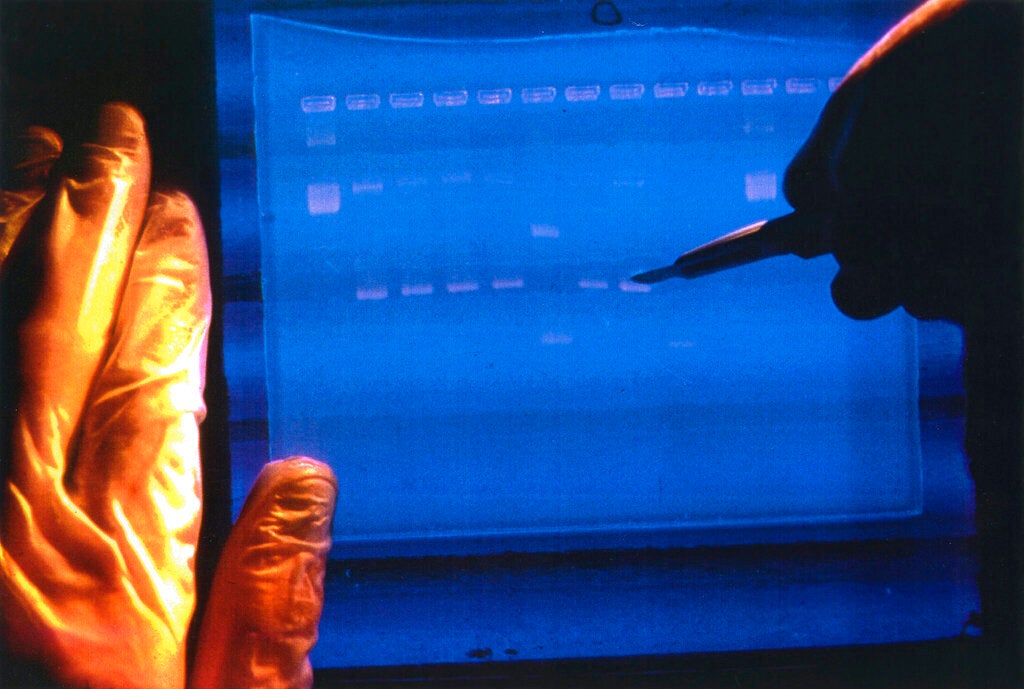
Dr. Steve Cho: Radiopharmaceutical therapies have been around for a while, going back to the 1930s when Iodine 131 was used to treat thyroid cancer. However, there has been a recent explosion in this area with advances in treating neuroendocrine prostate cancer causing a lot of excitement.
KAK: The University of British Columbia received more than $23 million to develop new radiopharmaceutical therapies. And the announcement was really bold, saying that nuclear medicine can cure cancer. What is your response to a claim like that?
SC: That announcement really underlies the excitement in the field and new developments in effectively treating cancer. In the clinical and research fields, we’re very cautious about using the term “cure.” But I do think this is one step in our effort to cure cancer. I don’t think we’re there yet, but I do think these new radiopharmaceutical theranostics are a step toward getting there. Currently, these therapies provide durable cancer remission and prolonged survival and quality of life for patients.
Prostate cancer is the second leading cause of cancer in men in the United States and second leading cause of death. There’s a treatment approved last year that has demonstrated effectiveness for (prostate cancer) patients.
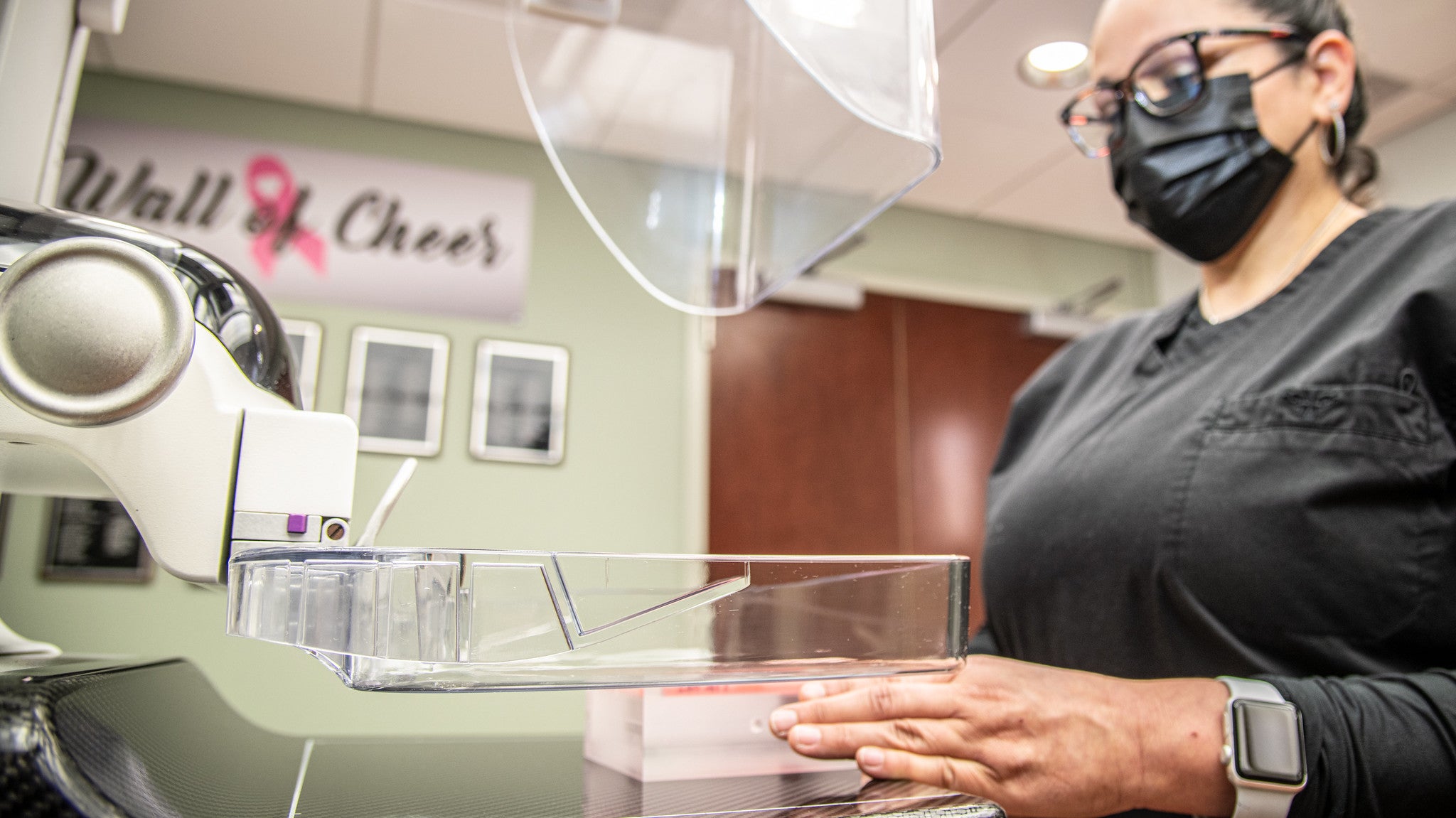
KAK: Your specialty is nuclear or molecular imaging to evaluate how organs function. Other imaging methods assess how an organ looks.
SC: Instead of a CT (computerized tomography) scan or MRI (magnetic resonance imaging) to look at the density of soft tissue and bone or water density in your body, molecular imaging uses radioactivity, molecular pathways and metabolism. We do it for cardiac and neuroimaging.
What radiation oncologists typically do is provide external beam radiation — high energy radiation from outside the body which they can contour and shield normal organs and target tumor cells for treatment.
KAK: An element of nuclear medicine, radioisotopes, have been in a global shortage recently. How has that affected your work?
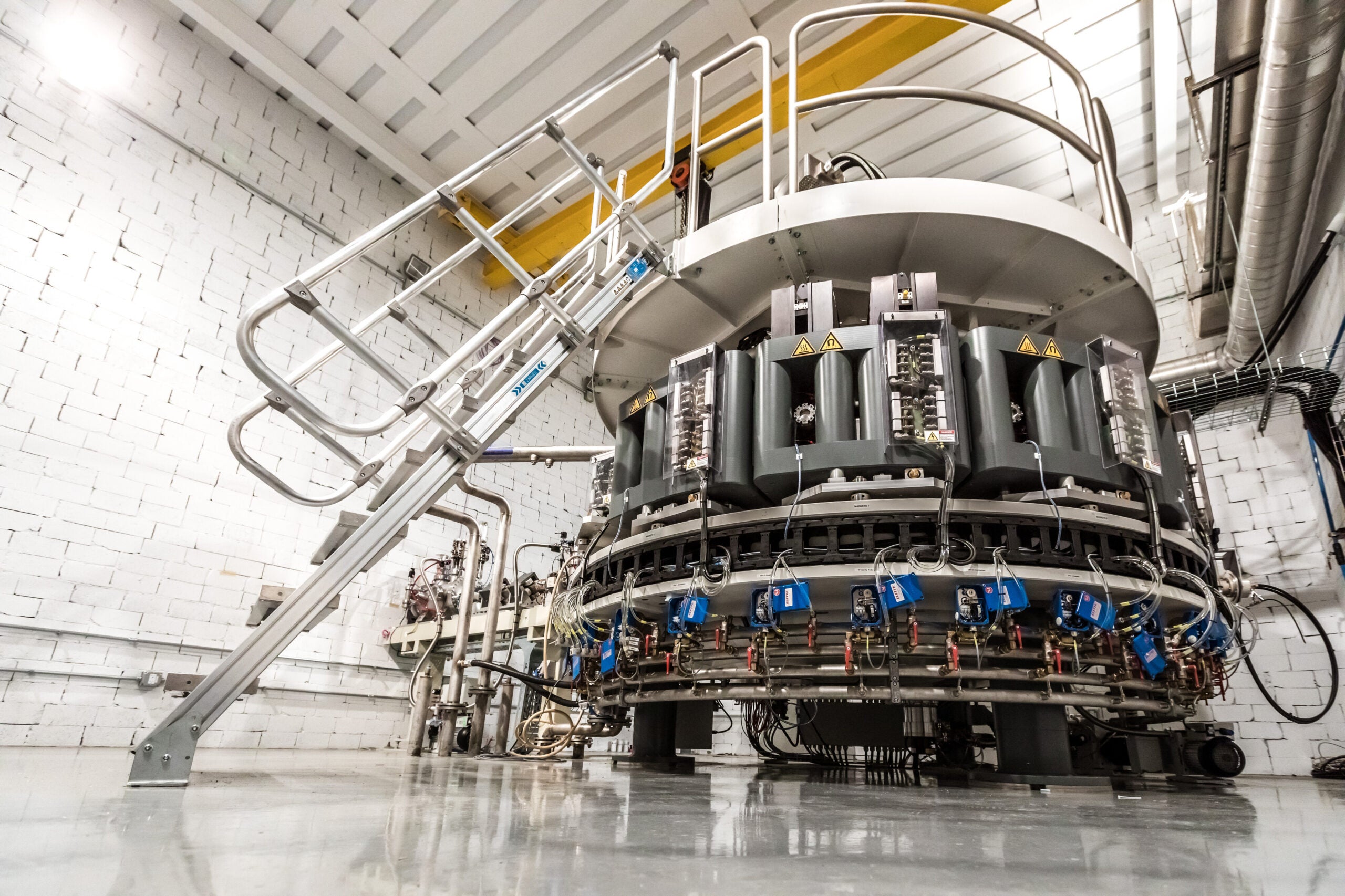
SC: There have been shortages in radiopharmaceuticals, both for imaging and for treatment. Technetium, the workhorse of nuclear medicine imaging radiopharmaceuticals, is made in several reactors around the world. There’s a limited supply when one of these reactors goes offline, either for renovations or unplanned production limitations. So that’s affected us. Some of the production that’s happening with NorthStar Medical Radioisotopes and SHINE Technologies in southern Wisconsin promises to help alleviate some of that in the future.
KAK: Patients are exposed to radioactive materials when they undergo a procedure using nuclear medicine. Should patients be concerned about the long-term risks of nuclear treatment?
SC: As with any treatment, we educate patients in coordination with their radiation safety officers. It’s not something they need to be inordinately concerned about if they’re following precautions. Many of these are typical of COVID precautions.
Radioactive (material)…comes out of the body in urine or stool, so we recommend good hygiene. And then its maintaining distance between the patient and other loved ones for a specific period of time depending on the radiopharmaceuticals. If you follow those precautions, your loved ones and the people around you and the public are very safe.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.