A new program to treat traumatic brain injuries in veterans and first responders is coming to Froedtert and the Medical College of Wisconsin following a $12.5 million donation from a national nonprofit.
Advocates for the program, known as Building Resilience through Action in Veterans and First Responders and shortened to BRAVE, say it’s the first of its kind in the Midwest.
“This new program … will accelerate our capacity to diagnose and treat traumatic brain injuries, post-traumatic stress disorder, and other conditions that we see far too often among our military veterans, their spouses and the families of emergency first responders,” Medical College of Wisconsin President and CEO John Raymond said during a press conference Thursday.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
The nonprofit Avalon Action Alliance, which aims to help veterans, first responders and their families, gave the Milwaukee-based hospital system the $12.5 million gift to help start the program. Avalon CEO Joe Brennan said typically, a patient diagnosed with a mild traumatic brain injury will have to go to appointments over an 18-month period. That can include visits with clinicians, physical therapists and behavioral health professionals.
The BRAVE program accelerates that process, as eight clinicians review medical records and schedule several clinical appointments through an outpatient program over a three-week period. Brennan said providers in the program will also tailor their therapies to patients’ needs.
“(The clinicians) don’t ask you what’s going on,” Brennan said about the program. “They ask what are your goals, how do you want to get better, what are your top priorities.”
The BRAVE program will conduct detailed clinical evaluations and develop a customized treatment plan specialized for an individual’s needs, according to a press release announcing the plans.
“You leave with an extensive follow-up plan,” Brennan said.
While veterans and first responders are not the only people who suffer traumatic brain injuries or post-traumatic stress disorder, data show they may be unusually prone to such injuries in the course of their work. A 2017 study found that 76 percent of firefighters report at least one brain injury in their lifetime. The National Alliance on Mental Illness estimates that 35 percent of police officers suffer from PTSD. Firefighters and police officers are also more likely to die by suicide than in the line of duty.
Milwaukee Fire Chief Aaron Lipski said his firefighters often go to Froedtert and the Medical College of Wisconsin with brain injuries. He praised the new program, calling it “solution-oriented.”
There are 331,000 veterans living in Wisconsin now. The U.S. Department of Veterans Affairs said PTSD is slightly more common among veterans than civilians and in some studies, PTSD is three times more common among veterans who deployed than in those who did not, because those deployments may have involved exposure to combat or other potentially traumatic experiences.
The Mayo Clinic found that symptoms of PTSD can include “flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.”
A traumatic brain injury can occur from a sudden blow or jolt to the head, which often happens during traumatic events, including an accident, blast or fall. The VA found that “many people who get a (traumatic brain injury) also develop PTSD.”
Dr. Ben Weston, the director of medical services for the Milwaukee County Office of Emergency Management, said more than 9 out of 10 firefighters and emergency medical professionals in Wisconsin report experiencing traumatic events at some point in their careers.
“It’s a needed source of support,” Weston said about the BRAVE program. “It takes down barriers for our first responders to seek out traumatic brain injury, but particularly mental health, support. And statistics point to a major need there.”
Weston said there’s a need for the program not just in southeastern Wisconsin, but also across the state and beyond.
“Having a center like this, where these professionals can seek out care in a familiar, a comfortable, a supportive environment … is going to be really critical,” Weston said.
Brennan said often brain injuries or mental health struggles are “invisible.”
“Although it’s an invisible wound (and) you can’t see it, what you do see are the challenges someone has who does have traumatic brain injury,” Brennan said.
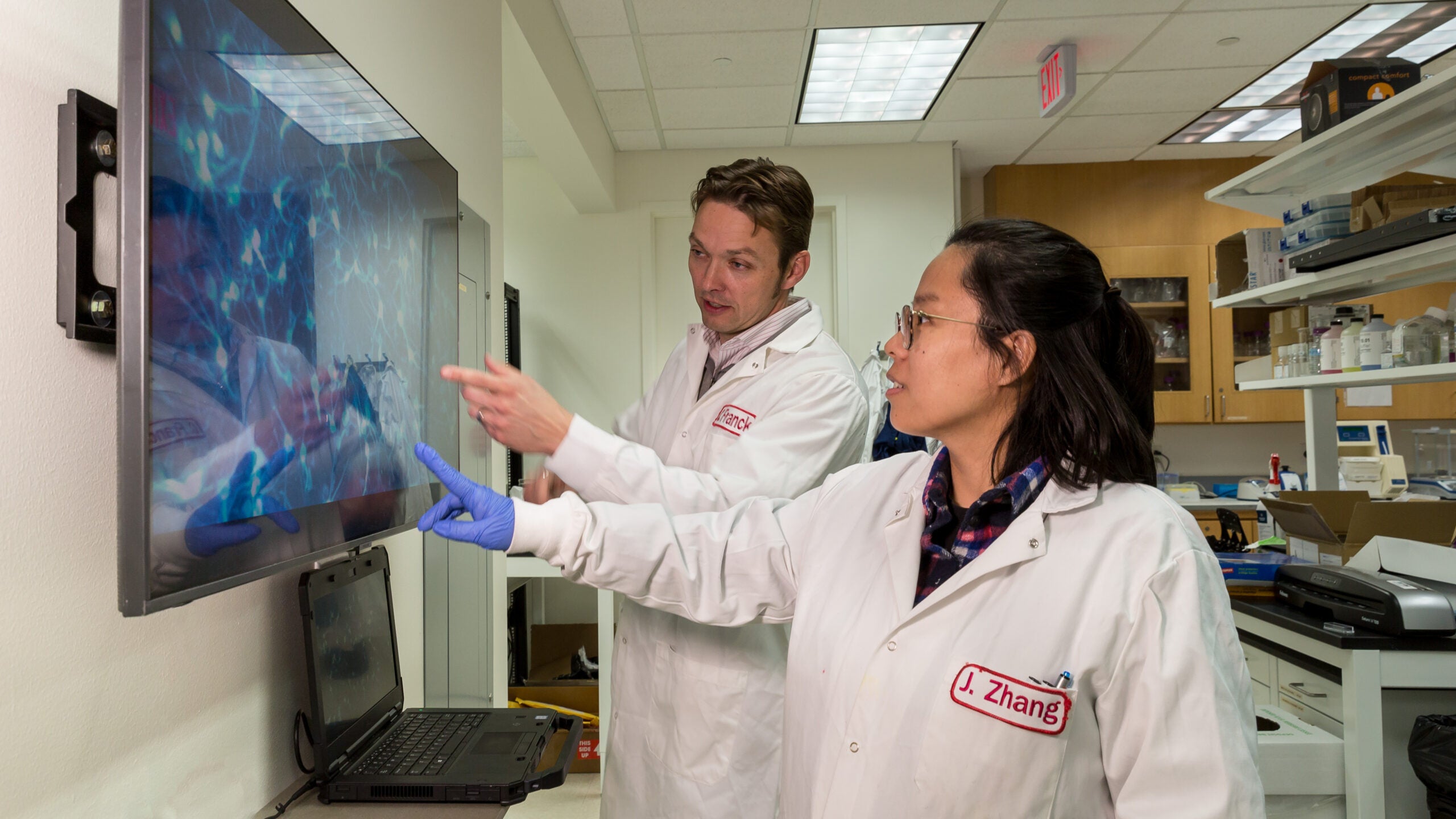
Michael McCrea, the director of Froedtert and the Medical College of Wisconsin’s BRAVE program, said that veterans and first responders often are placed in situations that result in “brain injury, trauma and great distress.”
“BRAVE will be designed to promote brain health and the restoration of brain health, through active therapies and by creating a culture in which injured veterans and service members regain the strength and resilience that led them to their calling to serve in the first place,” McCrea said.
Leaders at Froedtert and the Medical College of Wisconsin expect the hospital system to see national interest in the program. Five other programs across the nation currently participate in the BRAVE program.
“We expect BRAVE to be a destination for those in need across the country,” McCrea said.
The BRAVE program is expected to welcome its first patient this September at Froedtert and MCW’s Greenfield Highlands Health Center in Greenfield.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.