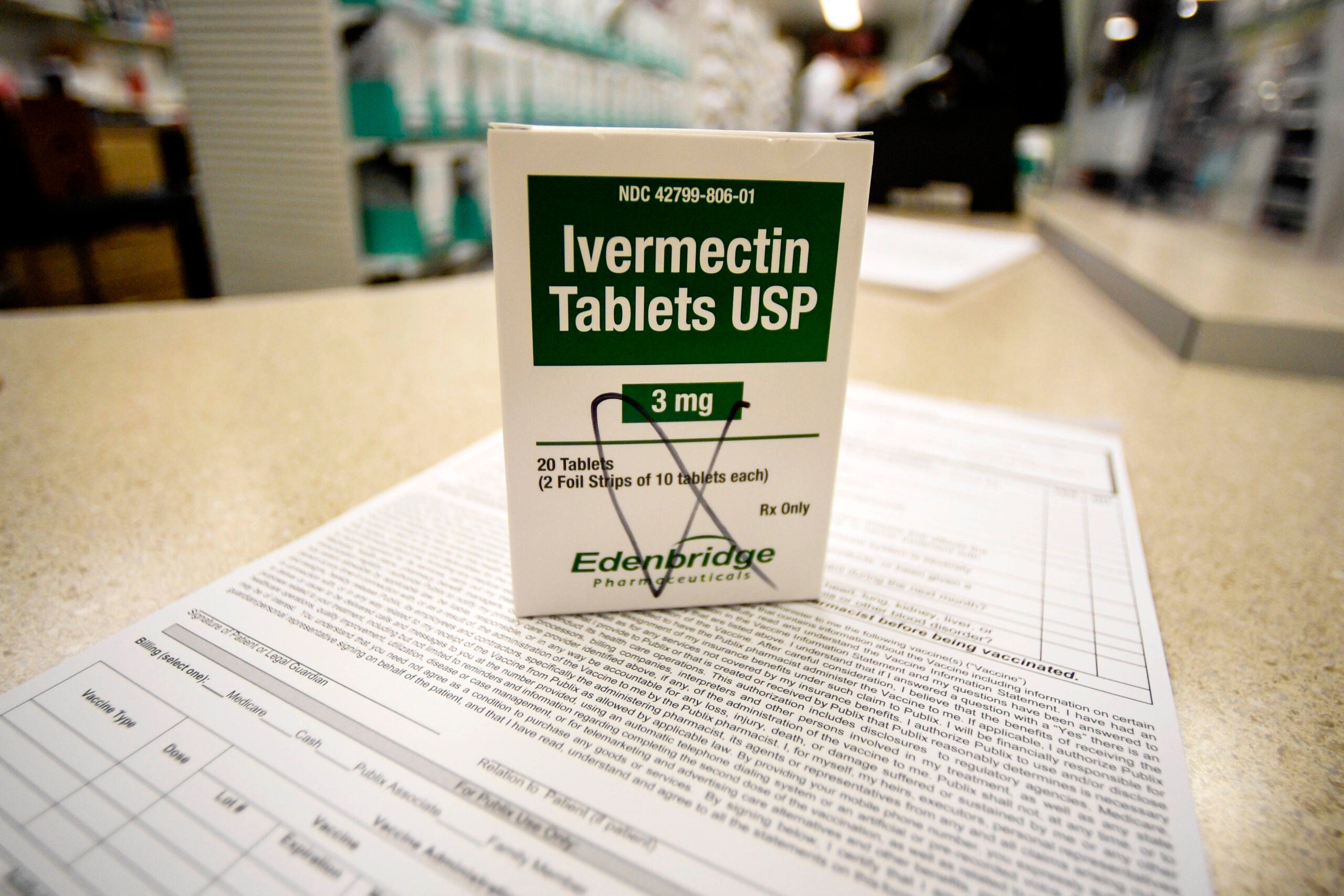
Ivermectin, a drug few people knew about before the coronavirus pandemic, has become so popular that health insurers are spending millions of dollars to fill prescriptions sought by doctors and their patients.
U.S. Sen. Ron Johnson, R-Wisconsin, and podcast host Joe Rogan have touted the drug as a way to prevent and treat COVID-19 — despite federal regulators warning against it this summer.
An analysis of pharmacy dispensing data by a University of Michigan researcher looked at a week in August when 88,000 prescriptions for the antiparasitic drug were filled, compared to only 3,600 prescriptions in a week for ivermectin before the pandemic.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
Dr. Kao-Ping Chua, from the University of Michigan Medical School, along with researchers from Boston University determined insurers in the United States spent $2.5 million on ivermectin for the week of Aug. 13, according to a study published in JAMA.
“There’s no reason to believe scabies and lice have increased 30-fold during the pandemic,” Chua said when asked what accounts for the sharp rise in use of the drug.
The analysis found insures may be spending nearly $130 million annually on the drug, which has not been approved by federal regulators to treat COVID-19.
Minnesota-based Mayo Clinic, which treats patients in Wisconsin, is not prescribing ivermectin for patients hoping to ward off the disease or treat mild symptoms, said Mayo Clinic Dr. Conor Loftus.
“The short answer is Mayo is not using ivermectin for this purpose,” Loftus said. “There has been no substantial evidence to date that ivermectin is effective for COVID-19.”
Ivermectin is part of a nationwide study on COVID-19 treatments which is being led by doctors at Duke University with funding from the National Institutes of Health. Loftus said if there is solid evidence in the future showing ivermectin or any other treatment works against COVID-19, the health system will consider using it.
Until then, authors who did the cost-analysis study published in JAMA say their findings suggest “insurers could prevent substantial waste by restricting ivermectin coverage; for example, by requiring prior authorization.”
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.