Science writer Sarah Zhang started covering COVID-19 for The Atlantic at about the time people in the United States first heard of the virus. In her myriad articles since, she’s explored microbes, how people say goodbye to dying loved ones via Zoom, and what it’s like writing about COVID-19 as a Chinese-American. Her latest stories have delved deeply into the newly-developed COVID-19 vaccines — how they work, the logistical and psychological challenges of the roll out, and what they mean for our society.
Speaking with “To The Best Of Our Knowledge” host Anne Strainchamps, Zhang shared what it’s like to cover a high-stakes, high-speed science story, and how what she has learned will inform her view of the year ahead.
This transcript has been edited for brevity and clarity.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
Anne Strainchamps: Sarah, what has surprised you most while covering the virus?
Sarah Zhang: What the whole pandemic has taught me is that science can move really, really quickly. We’ve learned so much about this virus in a year, but the things that really matter in public health — getting the public to listen and communicating — those things are hard. The science alone is not enough.
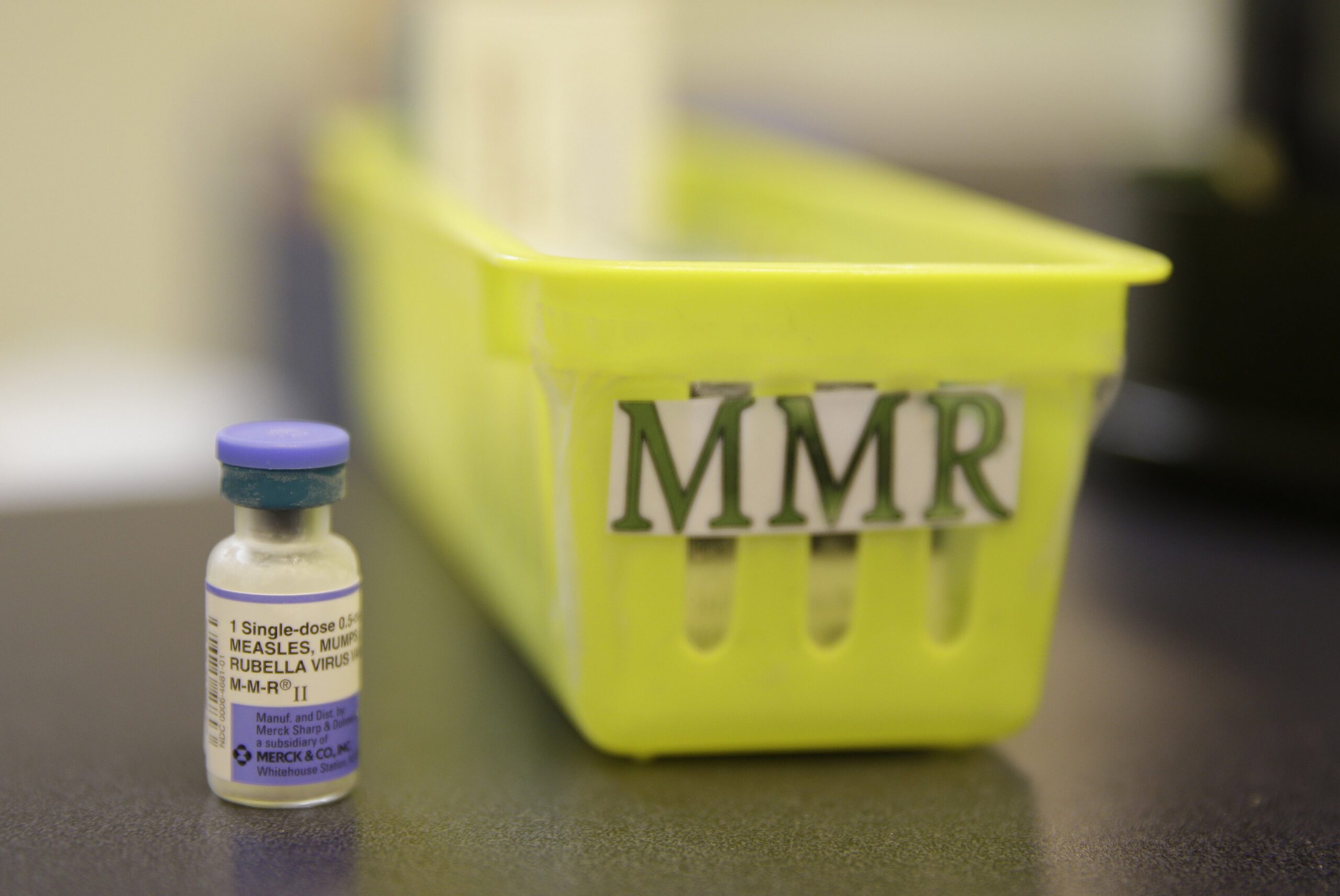
AS: The vaccine in production now — the mRNA vaccines — how are those different from the familiar standards? Smallpox, polio, diphtheria?
SZ: Traditional vaccines work by essentially giving you a little piece of the virus so that your immune system can recognize it. You might think of it as a “wanted” poster. So traditionally, this would be in the form of an inactivated virus, or a weakened virus, or maybe even just a fragment of virus.
mRNA vaccines actually give you the instructions to print out the “wanted” poster. The mRNA is basically a little molecule that has instructions for your body to make the spike protein on the outside of the coronavirus capsule — a really important piece of the virus (that helps it enter cells).
The way the mRNA vaccine works is that it’s encased in a little protective bubble of fat which helps get it inside your cells. Once the mRNA is inside your cell, it gives your body instructions to make that spike protein. And with that spike protein, your body’s able to recognize, “Oh, this is something foreign going on. Let me make antibodies against that. Let me stimulate the immune response against it.”
By the time you actually see the virus, it’s primed and ready to go. The instructions, the mRNA, disappear after a while. So does the spike protein itself. All you’re left with is this immune memory. So there’s no way to get sick, there’s no way to get COVID from getting the vaccine.
AS: Some people who’ve gotten the vaccine already have reported that there can be some — I don’t know if I want to call them severe side effects — but strong side effects, like worse than the usual sore arm you get from the flu vaccine.
SZ: Yeah, it has a bit of a kick. It stimulates a strong immune response, and that can feel like getting sick. When you get a fever, when you get a sore throat, when you feel achy, that’s actually all caused by your immune response. It’s not necessarily caused by the virus or the pathogen itself. So, the same thing is happening when you get a vaccine is that it stimulates the immune response.
AS: So is it actually a good sign? Does it mean that your body is developing the immunity? It’s working?
SZ: Yeah, it means that the immune system is gearing up and ready to do its job.
AS: And in the meantime, there’s not enough vaccine for everyone. Even those who can get it will need more than one dose before they’re fully immune. It’s not a magic bullet. You wrote this great piece recently talking about this period of time as “vaccine purgatory.” Can you explain what you meant?
SZ: Yeah, we’re about to enter this new phase where some people are going to have the vaccine, while other people aren’t going to have access to it. What you should do once you get the vaccine is a little bit unclear. How immune you are can vary person to person. So I think we’re just going to be in this period of flux where we’re waiting for a vaccine, but there’s not enough — I described it as purgatory.
As purgatory goes, I think one of the biggest questions is how long this is going to last. But as we’re seeing over the past month, it’s also going to take a long time to actually get these vaccines into arms.
AS: What would be your best case scenario for the people in the public health community? Would it be that the federal government just takes this over and the army moves in and sets up clinics everywhere and administers the vaccine?
SZ: I think it’s actually hard to say — that would certainly be very efficient, right? But if the army is setting up these vast mass vaccination clinics, are people going to trust that or do they prefer to get their vaccine from their local doctor’s office with a doctor they already know?
There’s a bit of a tension between doing things as quickly and efficiently as possible but also doing things the way that builds trust and feels fair. I don’t know if there’s really a right answer. And I think that’s part of what we’re seeing right now — every community is trying to figure it out for themselves.
AS: And then what happens if we wind up with some places, some states, some cities where everybody is vaccinated and there are other places where very few people are vaccinated?
SZ: Yeah, you’re right. We keep talking about herd immunity as if it’s a national thing. But it’s actually a local thing. Because it’s possible, as you say, to have everyone vaccinated in one town but in the next town over, there are still enough people who are vulnerable to COVID that an outbreak can break out.
The fact that we’re going to have this patchwork means that, first of all, I think COVID is so widespread that the virus is probably never going to go away. It’s going to be with us to some extent every year, like the flu. But you’re probably going to see bigger outbreaks in places where fewer people have been vaccinated.
And this just might be in addition to flu season — we’re going to have COVID season every year.
AS: It’s so strange to think about that and also to think about folks in Silicon Valley are all going to be super vaccinated before everybody else versus, you know, a neighborhood in Detroit. Do you worry about that kind of inequality?
SZ: Absolutely. I think one of the things that vaccine experts will talk about is that the people who can most advocate for themselves, who say they want the vaccine, are often not necessarily the people who most need a vaccine. The priority populations — people who are elderly, people who are frontline workers — are people who can’t get to a vaccine clinic or have to work during the day. They can’t take time off to go get the vaccine. If you’re elderly or homebound, how are you going to go out and get vaccinated?
So I think public health departments have a really big challenge in that the last 20 or 30 percent of people will be a lot harder than the first 20 or 30 percent of people.
AS: I’m thinking back over the big lessons of all of this, and the big challenges. One of them, it seems to me, is just how much uncertainty there has been this whole way through. And maybe that’s always true in science stories, but it’s a lot easier to handle the mystery of a black hole than the mystery of a virus that could kill you.
SZ: I’m so glad you asked that, because I feel like the past year has been about learning how to live with uncertainty and how to make decisions with imperfect information. I have gotten so many questions like, “Is this thing safe to do?” You know, “If I do this and this and this, can I go visit my grandparents?”
Maybe the way to think about this has never been is this “completely safe” or “completely not safe.” It’s always going to be “what is the amount of risk you’re willing to take?” It’s hard. It’s hard to say “we don’t know.” But it doesn’t mean we know absolutely nothing.
I mean, we have some amount of prior knowledge based on experience with other viruses, based on what we’ve known about how this virus spreads so far. So I think learning how to make decisions with imperfect knowledge is what we’ve all had to do over this past year.
And actually that’s what we’re doing all the time in our lives, right? It’s just that we often expect science to have a clear answer, and we don’t. And this is just a fact of life. We live with having to make decisions based on uncertain information.
AS: It seems like every time it feels like we’ve made some progress or there’s a reason to be hopeful, something else sort of smashes that down, like the second strain of the virus comes along. Are you still hopeful? How do you manage to stay that way?
SZ: Am I still hopeful? Well, I’m probably going to get married this year. We’re not going to have a big wedding or anything. But I think I am hopeful that our lives six months [or] a year from now are going to look quite a lot more normal than they are right now.
The vaccines, honestly, are just so much better than anyone really expected. I think that really did give me a good dose of optimism that there is an end to this. I’m clear eyed about the challenges ahead, but that’s just really wonderful news. And I think we should revel in that for a moment.
AS: I hope there will be an “it’s all over” moment. Do you have in mind even a little thing where you’ll feel like, “okay, it’s over”?
SZ: Yeah, probably when I eat inside a restaurant again and it feels normal. And I’m not worried about if everyone is wearing a mask.
I will probably get a vaccine this year. And I’m really looking forward to that.