New York City is the country’s largest hot spot for COVID-19 cases.
According to data from the New York City Health Department, as of April 8, there were over 80,000 confirmed cases, more than 20,000 people hospitalized and 4,260 deaths linked to the coronavirus outbreak that is sweeping across the country and the world.
The numbers continue to grow, dangerously stressing the health care system in New York City. As a result, both supplies and staff have come from across the country to help.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
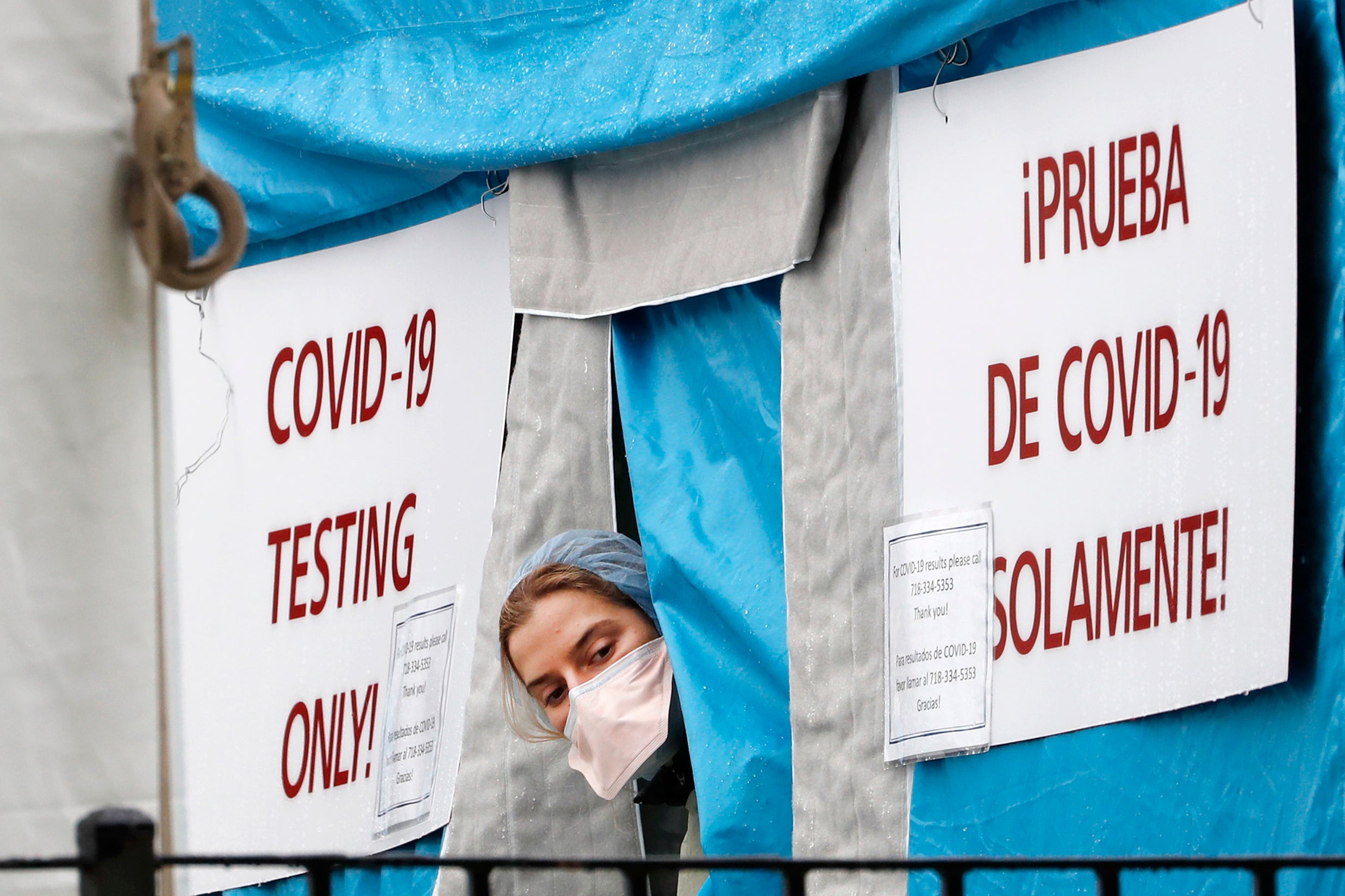
[[{“fid”:”1216986″,”view_mode”:”embed_portrait”,”fields”:{“format”:”embed_portrait”,”alignment”:”right”,”field_image_caption[und][0][value]”:”%3Cp%3EWisconsin%20nurse%20practitioner%20Jackie%20Christianson%26nbsp%3Btakes%20a%20break%20in%20the%20COVID-19%20tent%20hospital%20to%20document%20on%20her%20patients%20in%20New%20York%20City.%20%3Cem%3EPhoto%20courtesy%20of%26nbsp%3BJackie%20Christianson%26nbsp%3B%3C%2Fem%3E%3C%2Fp%3E%0A”,”field_image_caption[und][0][format]”:”full_html”,”field_file_image_alt_text[und][0][value]”:”Wisconsin nurse practitioner Jackie Christianson in the COVID-19 tent”,”field_file_image_title_text[und][0][value]”:”Wisconsin nurse practitioner Jackie Christianson in the COVID-19 tent”},”type”:”media”,”field_deltas”:{“1”:{“format”:”embed_portrait”,”alignment”:”right”,”field_image_caption[und][0][value]”:”%3Cp%3EWisconsin%20nurse%20practitioner%20Jackie%20Christianson%26nbsp%3Btakes%20a%20break%20in%20the%20COVID-19%20tent%20hospital%20to%20document%20on%20her%20patients%20in%20New%20York%20City.%20%3Cem%3EPhoto%20courtesy%20of%26nbsp%3BJackie%20Christianson%26nbsp%3B%3C%2Fem%3E%3C%2Fp%3E%0A”,”field_image_caption[und][0][format]”:”full_html”,”field_file_image_alt_text[und][0][value]”:”Wisconsin nurse practitioner Jackie Christianson in the COVID-19 tent”,”field_file_image_title_text[und][0][value]”:”Wisconsin nurse practitioner Jackie Christianson in the COVID-19 tent”}},”link_text”:false,”attributes”:{“alt”:”Wisconsin nurse practitioner Jackie Christianson in the COVID-19 tent”,”title”:”Wisconsin nurse practitioner Jackie Christianson in the COVID-19 tent”,”class”:”media-element file-embed-portrait media-wysiwyg-align-right”,”data-delta”:”1″}}]]Jackie Christianson is a nurse practitioner who traveled from Wisconsin to New York City to work in an emergency department during the COVID-19 pandemic. She had originally planned to take vacation time in April, but said she changed her mind as she saw what was going on.
“It seems silly for me to sit on the sidelines when there’s a crisis going on,” she said.
As a nurse practitioner, Christianson performs much of the routine health care that a doctor would in an average visit, like taking vitals, evaluating symptoms and diagnosing what might be ailing the patient.
But working in an emergency room in New York City during the coronavirus pandemic has been anything but a typical assignment, she said.
Christianson said that many people are coming in with respiratory distress — a hallmark symptom of COVID-19. One test that is performed uses a pulse oximeter, a device that measures the level of oxygen in the blood.
In a healthy person, Christianson said that the oxygen level would be between 96 and 100 percent. But in patients coming in with COVID-19 symptoms, “We’re routinely seeing people at 75, 80 percent, sometimes even worse,” she said.
Christianson added that “even with supplemental oxygen, we’re sometimes seeing them only come up into the low 90s.”
In addition to low blood oxygen levels, she said many COVID-19 patients are suffering from septic shock, a dangerous condition in which blood pressure drops dramatically, decreasing blood flow to major organs.
Christianson’s experience in New York has been full of ups and downs. She said there are moments when the teamwork is incredible and people are feeling good about the help they’re able to provide.
But she said there are real lows, too. The patient load for health care providers in the emergency room can be several times more than a normal assignment, which is both physically and emotionally exhausting.
“A normal patient ratio for nurses is about, maybe at most five patients in an emergency department for one nurse,” Christianson said. “The lowest ratio I’ve seen here is 12 relatively sick people for one nurse. We’ve seen ratios as high as 20, 25 patients for just one RN, and it’s just not enough.”
Even seasoned professionals can reach their breaking point under those conditions, she said.
“Sometimes, some of the nurses are in the nurses’ station, just in tears, because they can’t handle what’s going on. Nor should they handle what’s going on,” she said. “The resources, as far as manpower, are just absolutely stretched to their limits.”
After seeing the crisis firsthand in New York City, Christianson had this advice for reducing the risks and slowing the spread of the coronavirus in Wisconsin:
“If you don’t think that you’re in a life threatening condition, don’t come to the emergency departments. Most of the people that we’re seeing are coronavirus patients that are sick enough that they do need medical intervention,” she said. “But we’re still seeing some people come in for things that they honestly don’t need to be seen for on an emergent basis. And they’re exposing themselves to all the other coronavirus patients when they do come in. So please, if you can help it, stay home. Self-manage at home. Do the best that you can to avoid leaving your house if you are sick.”
Those who are interested can follow Christianson’s experiences in an online journal she is keeping during her time in New York.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.