Time has taken on elastic qualities over the course of the COVID-19 pandemic— slowing, stretching and slipping as uncertainty has reigned — but its passage has been accompanied by one abiding hope: finding a remedy. Medical researchers around the world have spent their time on parallel yet overlapping quests to take on the disease — through better testing, more effective treatment and ultimately vaccination.
In Wisconsin, scientists have been in the thick of research into the coronavirus and ways to fight its spread and effects. Their work has contributed to ongoing efforts to develop multiple vaccine candidates, as well as improvements in treating those who have fallen ill with COVID-19 and identifying those who are infected. All of these tracks are priorities, and although the first deployment of vaccine doses is raising hopes that a resolution is within sight, the pandemic will not end overnight.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
The coronavirus that causes COVID-19 is novel, but the urgent pursuit of unlocking the mechanisms of an unfamiliar virus is not new.
About four decades before COVID-19, another unknown disease caused by a virus changed the world — AIDS, caused by HIV, has been the focus of intense research since the virus was identified.
There were optimistic forecasts about how long it would take to develop treatments for HIV, but it has claimed many millions of lives, and took decades to only partially contain. As that pandemic stands, a patchwork of treatments and preventative measures are still required to combat HIV and slow the spread and course of AIDS.
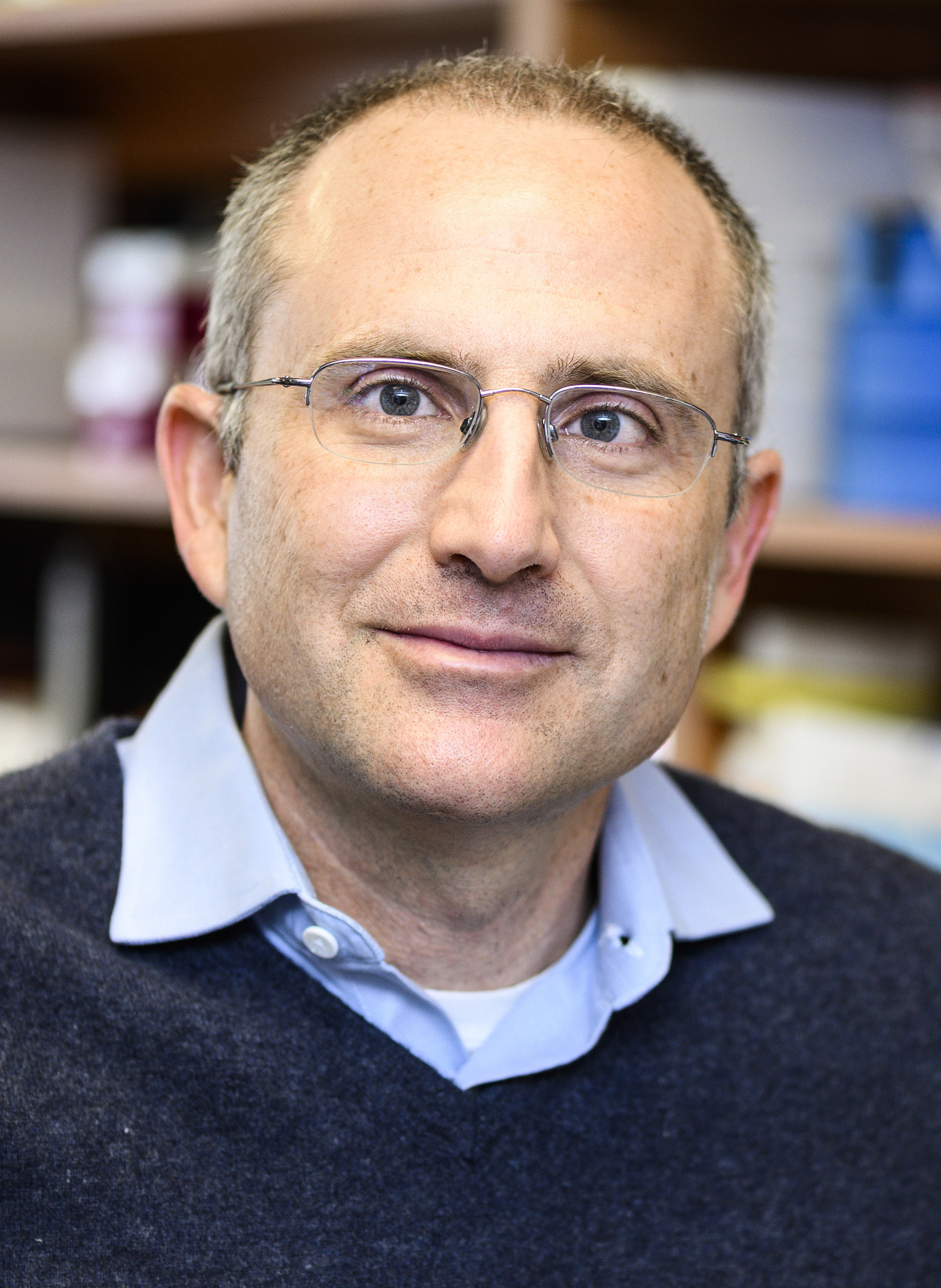
David O’Connor, a professor of pathology and laboratory medicine at the University of Wisconsin-Madison, has spent much of his career studying HIV, leading a lab studying that virus and other emerging pathogens. While the distribution of COVID-19 vaccines expands, he cautioned that it is only one tool for fighting a pandemic that will likely require an entire toolbox of tactics.
“It’s not going to be like the movies Contagion or Outbreak. You’re not going to suddenly have the vaccine and then everything returns to normal the next day,” O’Connor said.
Exactly when COVID-19 will ultimately be contained remains uncertain, but the public health and medical communities have committed to a similarly intense response.
A need for treatments
Even as the COVID-19 vaccine candidates progressed toward their first patients over the fall of 2020, Wisconsin-based scientists have continued working to develop strategies to contain COVID-19. In addition to participating in a vaccine trial coordinated by Oxford University and AstraZeneca, researchers are contributing to the manufacturing of coronavirus treatments, and improving testing practices as part of ongoing efforts to address public health and safety.
William Hartman, the principal investigator for the AstraZeneca vaccine trial being conducted at UW-Madison, pointed to the university’s research capacity and infrastructure to support large-scale clinical projects developed to respond to the pandemic. Where vaccines and treatments usually take months or years to reach a trial stage, Hartman underscored the immediate need for research to combat COVID-19, which had only a matter of weeks to get underway in the spring.
One reason COVID-19 was able to spread quickly with devastating results is that it is a previously unknown coronavirus — SARS-CoV-2 — and therefore options for effective treatment had to be developed and tested from scratch.
One treatment option is the use of convalescent plasma, wherein a person who has recovered from an infectious disease donates antibody-rich blood plasma to an infected patient to help them fight the illness. In late August 2020, the U.S. Food and Drug Administration granted an emergency use authorization for the use of convalescent plasma in treating COVID-19. This treatment started being manufactured in September for clinical trials.
According to Carl Ross, the director of Waisman Biomanufacturing, this treatment technique is not without drawbacks, particularly the need to use donated plasma.
“If you go and give blood now, they’ll automatically do a test for [COVID-19] antibodies and they’ll be really happy if they find that you have [them],” Ross said. “The disadvantage of that type of treatment is that you have to get plasma from people, so that’s obviously rate limiting. And it’s also not necessarily consistent.”
Seeking to overcome these practical limitations, researchers at the California-based biotechnology company GigaGen are working to develop an antibody treatment that functions like blood plasma but can be grown in a lab with consistent specifications. Waisman Biomanufacturing, which is affiliated with the Waisman Center at UW-Madison, partnered with the firm to supply the trials of a newly developed drug named GIGA-2050.
The drug is produced in a bioreactor (a general term for a system that grows organisms, such as fermenters and corn ethanol stills). In this case, a bioreactor grows antibody cells in a liquid medium. A large system will be able to manufacture thousands of liters of the antibody treatment at a time, and while the amounts prepared for the GIGA-2050’s clinical trials are comparatively smaller, Ross said the drug would be manufactured in volumes larger than are typical for early stages of testing.
The speed at which researchers are advancing work related to COVID-19 has helped fuel distrust motivated by safety concerns when a vaccine or course of treatment is made widely available.
Ross explained GIGA-2050 would undergo the same clinical trial process as any other drug, and said hazards associated with shortened development timelines are economic gambles taken by the companies conducting the research.
“Most of the difference is that we’re taking calculated risks in the development,” Ross said. “You don’t like to go into a large production reactor before you really fully characterize and develop the process at a small scale, because running that big reactor is expensive and time consuming. But in this case, we have to get to the big reactor quicker.”
The AstraZeneca vaccine trial paused in the U.S. as the FDA and National Institutes of Health reviewed an adverse event in a participant that occurred in the United Kingdom. Hartman called this action a sign that officials in the U.S. took appropriate precautions to ensure the trial could resume safely, which it did in mid-October.
The FDA also plays a role in increasing the speed at which vaccines and treatments are developed. Although the approval process and requirements remain the same, the agency has prioritized work related to COVID-19. At regulatory agencies, universities and other research institutions, and among pharmaceutical companies around the world, resources have been shifted to an exceptional degree in response to the coronavirus.
“Never before has such an effort, from a people side and from a money side, come together in such a focused way to develop anything,” Hartman said. “While the speed is unprecedented, so is the effort.”
Accelerating testing
As long as the coronavirus continues to infect people on a widespread basis, testing bottlenecks remain a barrier to containing COVID-19. Although tests became generally available within a couple months following the early weeks of the pandemic, the number of people seeking tests also grew as the virus spread.
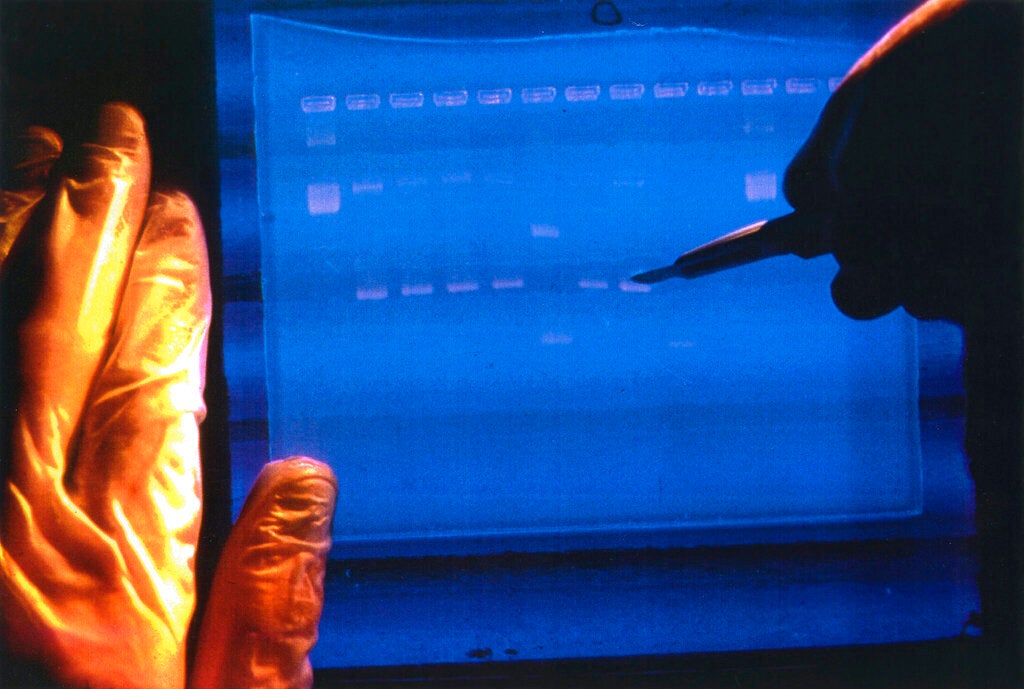
As UW-Madison researcher David O’Connor explained, the greatest potential for lag shifted from testing sites to the laboratories where samples are processed. The primary type of COVID-19 test being administered uses polymerase chain reaction, known as PCR methodology, to detect the presence of viral RNA in a subject’s mucus or saliva. This type of test must be processed in a lab outfitted with expensive equipment and specialized staff, which has led to delays in results at certain points in some areas.
O’Connor said eliminating delays and increasing the availability of tests that deliver same-day results is critical in slowing spread of the virus.
“If you are contagious today, you should be isolated today, not tomorrow, not a week from now,” O’Connor said.
To achieve this goal, O’Connor’s lab has been researching another way to pinpoint COVID-19 infections using loop-mediated isothermal amplification, or LAMP.
LAMP testing functions similarly to PCR by detecting viral RNA in a subject’s fluid sample but requires less intensive processing and corresponding training to conduct. Its widespread availability could allow for more regular, rapid testing in workplaces, schools and other potentially crowded locations where the coronavirus would easily spread from infected individuals.
O’Connor noted antigen testing, which detects the presence of the coronavirus surface proteins, serves as a rapid diagnostic tool, potentially with a function similar to an over-the-counter pregnancy test.
Although LAMP and antigen testing can be less sensitive than PCR when detecting individuals who are positive but have a low viral load, O’Connor said their sensitivity improves when spotting those with high viral loads who are most likely to be contagious.
He stressed that more widespread testing, along with common measures like mask use and distancing, remain the best way to limit infections in advance of the widespread administration of an effective vaccine.
“These need to be linked together as part of a continuum where people wear masks and they keep their distance, and you use testing to identify people who are contagious and take them out of circulation so that they’re less likely to infect other people,” O’Connor said. “Right now, each point within that continuum is really stressed.”
Given the lead time for the distributing COVID-19 vaccine supplies, O’Connor said testing fatigue may become a challenge if regular checks for coronavirus among seemingly healthy populations are widely adopted. He said support and encouragement within communities and a normalization of testing procedures and other prevention measures could help assuage frustrations that arise with an ongoing public health crisis.
That aspect of community buy-in, or lack there-of, as has been the case with masking, is also likely to play a major role in the success of vaccines when they’re made widely available.
UW-Madison researcher William Hartman said predictive models suggest 70-80% of the population will need to get a vaccine to fully contain COVID-19. With many people voicing their intent to refuse vaccination, he said researchers must make a compelling case for why this prevention practice is important.
“It’s our job to show that these trials are being done correctly, safely, and to see where people want us to enhance the education and promotion of these vaccines so that they can feel comfortable receiving it moving forward,” Hartman said. “Ultimately, it’s a free country. People are allowed to accept the vaccine if they want. They’re allowed to deny it if they want. But to get us to a normal place again, we need to get as many people vaccinated as possible.”
The promise of vaccines
When the Oxford AstraZeneca vaccine trial was paused in September, some participants in Wisconsin had already received a dose. While confidentiality rules limited the ability of UW’s trial’s principal investigator William Hartman to comment on the specifics of that stoppage, he expressed confidence in the protocols that underpin the vaccine’s development.
UW-Madison is among many research institutions participating in trials for the various COVID-19 vaccines being developed and rolled out around the world. As of September 2020, the Oxford AstraZeneca trial included 80 sites around the world, and had recruited around 30,000 participants.
Although these trials share the goal of neutralizing the threat posed by COVID-19, they differ in approach and biological composition. The vaccine being tested at UW-Madison uses a chimpanzee adenovirus — modified to prevent transmissibility in humans – embedded with the genetic material of the SARS-CoV-2 spike protein that allows the virus to bind to human cell receptors, prompting an immune system response to that protein.
This approach was also used to develop vaccines for SARS and MERS, other coronaviruses with the potential to severely impact human health that emerged in 2003 and 2012, respectively. The outbreaks associated with SARS and MERS were contained with comparative speed, however, and vaccines in development for the viruses never reached distribution at those points.
Other COVID-19 vaccines in development utilize more experimental methods. The vaccine developed by biotech firm Moderna uses the virus’s own RNA sequence that would, ideally, prompt the same immune response, without the need to use an intermediary virus.
Hartman said this approach may allow for faster development of vaccines, but the underpinning technology is new, and the technique has been untested.
Peter Halfmann, a senior scientist at the UW-Madison Influenza Research Institute, said the intermediary virus and RNA approaches differ somewhat from other contemporary vaccines that are routinely given for mumps, whooping cough and other diseases. Many common vaccines are created from virus cells that have been killed or modified to limit replication.
Halfmann explained these differences in design and composition can influence a vaccine’s effectiveness and the longevity of the immunity it confers. A vaccine that uses an adapted virus will tend to prompt a strong immune response that closely mimics how the body would react to the live virus, but this process may pose problems for recipients who are immunocompromised.
Halfmann predicted early versions of vaccines for COVID-19 will be relatively weak, some requiring multiple doses to confer effective immunity — indeed, the Pfizer vaccine is administered in two doses. Hartman indicated the Oxford AstraZeneca trial and others may continue even after vaccines are made available to the public, in order to monitor long-term effectiveness.
“We bring those subjects back periodically over the next two years to evaluate what their antibody level is, to make sure that they’re still immune to the disease or whether or not they need to have some sort of a booster,” Hartman said. “While a vaccine may be available, all the information that we need from those will not be available yet.”
The process of long-term evaluation of vaccine effectiveness has led to ethical questions over whether trial participants who were given a placebo or doses of a COVID-19 vaccine found to be ineffective will be able to receive a different vaccine.
While work on different ways to contain and eradicate COVID-19 is making swift progress, researchers continue to make discoveries about how the coronavirus infects and spreads, continually injecting uncertainties to development timelines and the potential effectiveness of any one approach. With many people pinning hopes for a return to normalcy on the protection offered by vaccines, demands to distribute COVID-19 vaccines as soon as they are produced are setting their own timeline.
O’Connor recalled a similar clamor about another virus.
“When the virus for HIV was first discovered, the secretary for Health and Human Services, Margaret Heckler, announced that there would be a vaccine for HIV available in 18 months… now we are nearly 40 years later and we still don’t have an effective vaccine,” O’Connor said. “There are good biological reasons why it should be easier to make a vaccine for this virus than for HIV, but we don’t have one.”
Hopes and demand are high for the emerging COVID-19 vaccines, but given the time needed for production and distribution, the potential for refusal among many people, the simple fact that the pandemic remains serious as the virus spreads through the dark of winter. Patience will be another demand over this time, even as researchers continue their work on different ways to address the crisis.
“We need to be prepared for any eventuality,” cautioned O’Connor.
This report was produced in a partnership between Wisconsin Public Radio, PBS Wisconsin and the University of Wisconsin Cooperative Extension. @ Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.