Wisconsinites may find themselves in new territory, trying to navigate a path forward through the difficult and uncertain terrain of the COVID-19 pandemic. While adjusting daily routines and doing business in such unique circumstances certainly requires adaptability, looking back at how previous public health emergencies unfolded can offer insights on what’s happening today.
The 1918 influenza pandemic and how the ordeal played out in Wisconsin illuminates the scale at which the experience of and response to public health emergencies impact both human lives and the economy.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
Also known as the “Spanish Flu,” due to early news coverage of the disease in Spain, the 1918 pandemic hit Wisconsin in the fall of that year, just before the end of World War I. Nearly 103,000 Wisconsinites fell ill with the H1N1 influenza and related pneumonia, with over 8,000 losing their lives — a total greater than the number of people from the state who were lost in World War I, the Korean War and Vietnam War combined. Globally, the 1918 flu claimed 20-100 million lives, depending on the estimate.
Wisconsin was the only state in the nation to respond to the pandemic with measures that were both particularly aggressive and well-followed by the public. The state laid the foundation for this comprehensive approach decades earlier. Wisconsin was an early adopter of several public health practices, including implementing a State Board of Health in 1876, the precursor to the Department of Health Services. It was only the tenth state to do so.
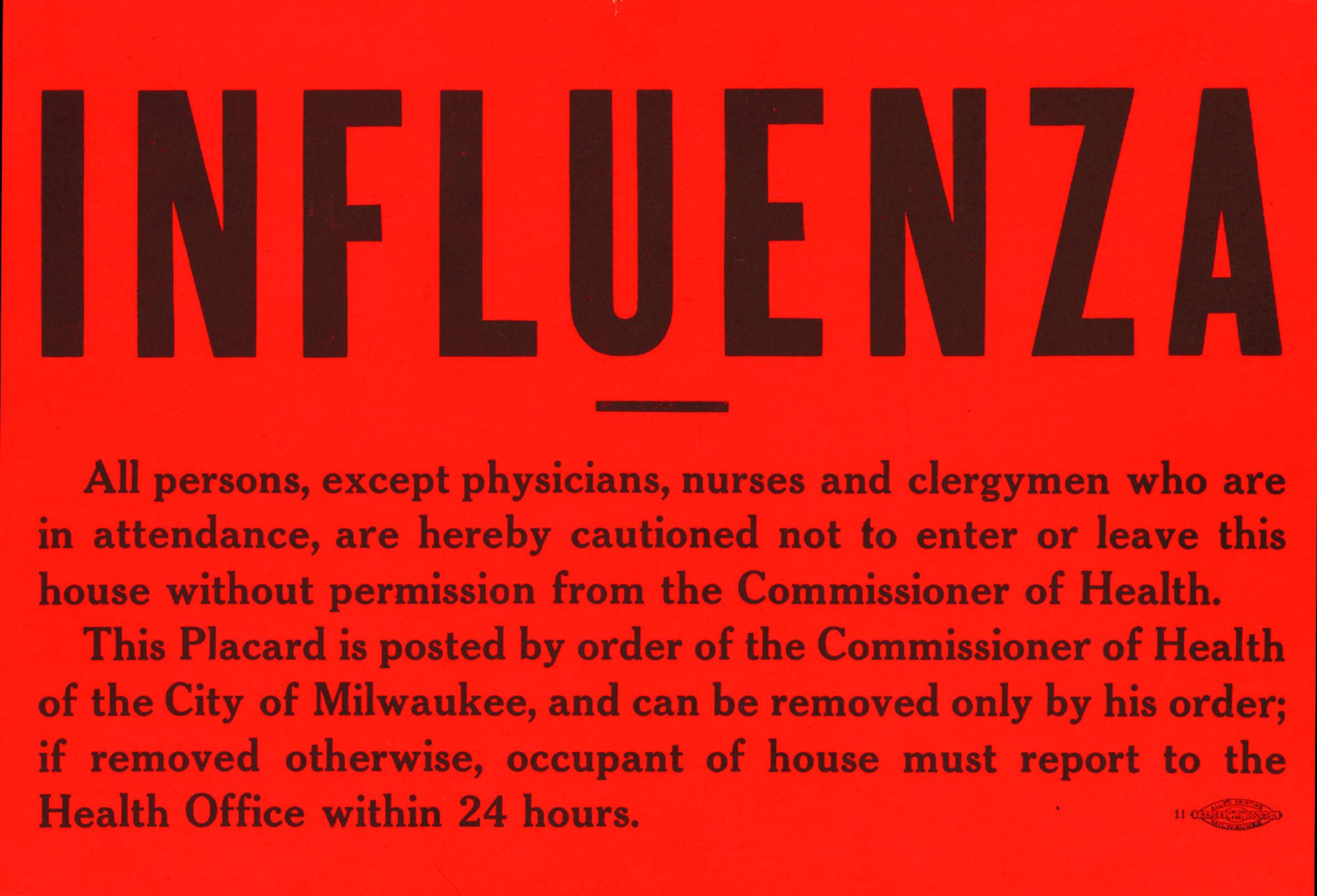
During public health emergencies, the board was granted power to implement quarantines and issue rules and regulations for the state in the interest of public health. Not long after establishing the board, the state also required that all localities (cities, villages and townships) create a local board of health and appoint a public health officer. At the time of the 1918 flu, nearly 1,700 local boards of health existed to bridge individual communities to the State Board of Health and enforce local regulations.
Much like the COVID-19 pandemic, the 1918 flu interrupted routine life in Wisconsin. Large gatherings posed a risk of spreading infection, and the public was directed to avoid crowded venues. Eventually, the State Health Officer, a member of the State Board of Health, ordered all public institutions in the state to close. Further, at the direction of that official, local governments were ordered to close all movie theaters, schools, churches and public gathering spaces indefinitely. Nearly all localities cooperated within a day.
Wisconsin was the only state to issue such comprehensive statewide measures.
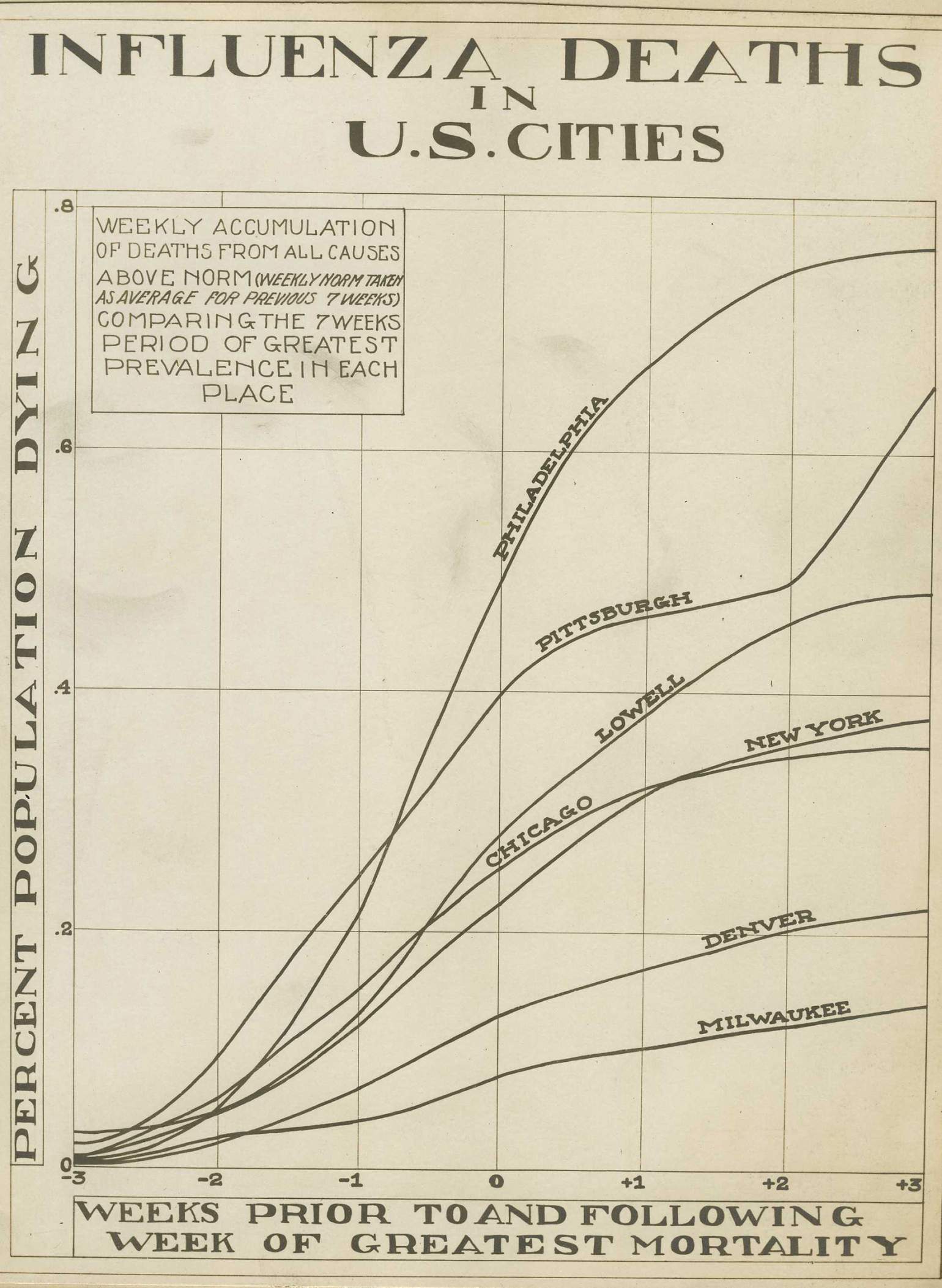
This state-level approach and public compliance, combined with low population density and the relatively late arrival of the flu, is credited with the relatively low death rates for Wisconsin in 1918. Indeed, flu mortality rates had little relationship to states’ economic conditions, climate and geography, perhaps further suggesting Wisconsin’s government intervention played at least some role.
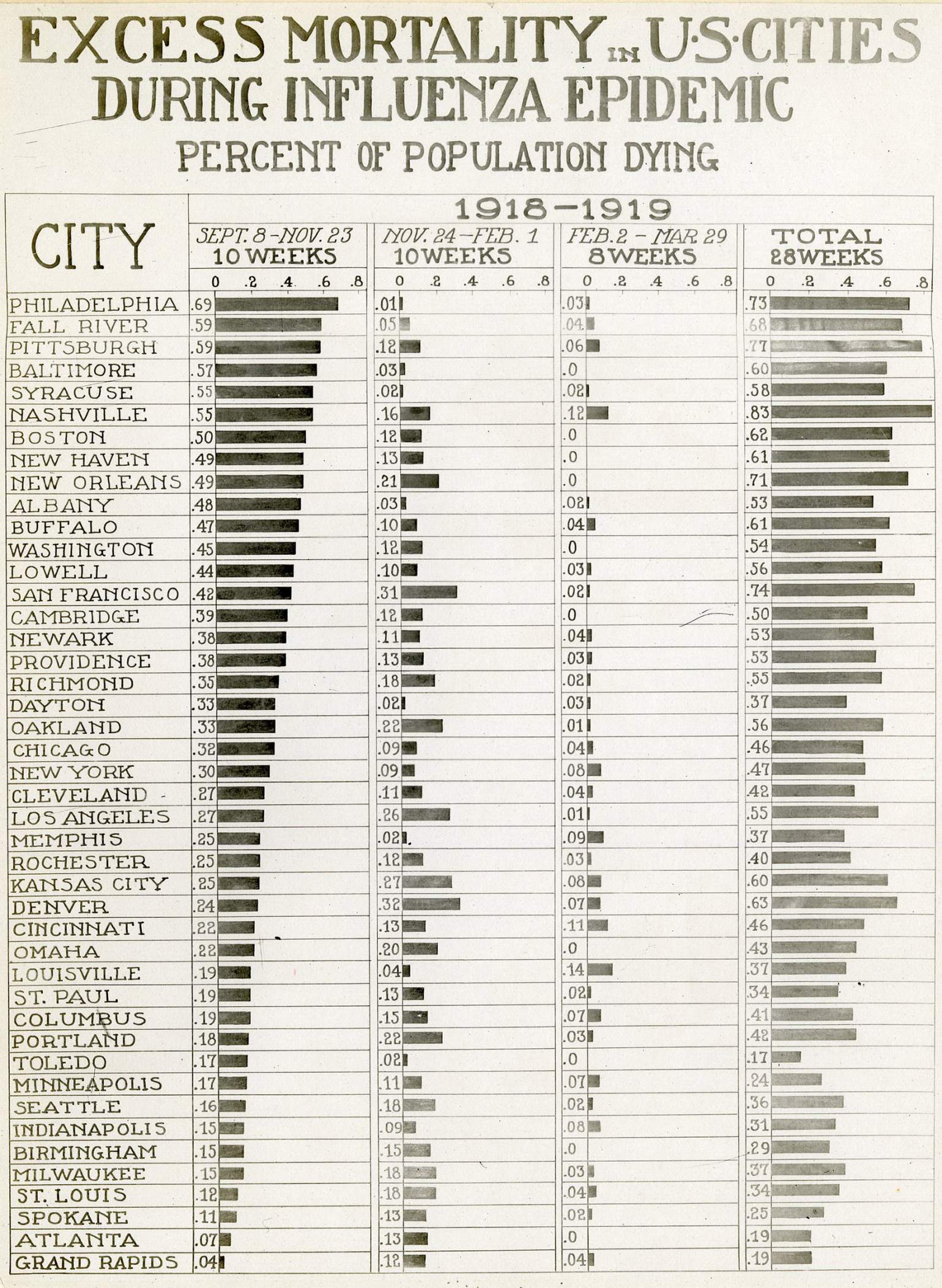
The death rate in Wisconsin was 2.91 per thousand compared to 4.39 per thousand in the rest of the United States. Alternatively, one study found a death rate of 3.3 per thousand for the state — the third lowest among 25 reporting states — compared to 4.8 per thousand nationally for just the four months between September and December 1918. Yet another analysis ranked Wisconsin as having the lowest mortality rate of states reporting in the U.S. that year.
The excess mortality rate — which refers to deaths beyond what would be expected during a typical flu season — was one of the lowest in the nation at 360 per 100,000. Milwaukee had one of the lowest death rates of all cities of its size.
In addition to these relatively low mortality rates partly attributable to the intervention strategy in Wisconsin, a 2020 study suggests there may be economic benefits. The economies of cities that intervened sooner and more aggressively performed at least as good if not better once the pandemic was over.
The consequences in 1918
Despite the uniquely coordinated efforts at the state and local level, hospitals throughout Wisconsin faced a shortage of beds and healthcare workers. Communities augmented their capacity with temporary emergency facilities and a network of volunteers. Locally, many places participated in anti-influenza education encouraging people to stay home when sick and cover their cough.
Wisconsin’s rural and urban areas faced, to some extent, different challenges in dealing with the 1918 flu pandemic. In more urban places, the number of patients overwhelmed healthcare systems and limited access to quality care. In rural areas, scattered populations and limited resources to channel toward education and public initiatives left some people dangerously uninformed. Rural areas across the nation, though, did fare better as indicated by lower rural mortality rates across several states and compared to state averages. In Wisconsin, the ratio of the mortality rate for cities compared to the state average was 1.17; that is, the urban mortality rate was 17% higher, indicating that rural areas likely had fewer flu-related deaths.
The 1918 pandemic ultimately proved most severe for prime age adults — peaking from ages 15 to 35 with higher mortality rates for males. For many households, the loss of a breadwinner, even for only the two weeks necessary to recover, was crippling. Many families suddenly found themselves in dire need of assistance.
Civic life changed as well, as the outbreak hindered public campaigning events, causing political parties to largely switch to mail outreach. Businesses suffered too. Movie theaters, restaurants, bars and saloons missed months of revenue. Unsurprisingly, healthcare-adjacent businesses, such as equipment manufacturers and other suppliers, experienced growth. Beyond those businesses forced to close, many faced worker shortages when broad swaths of the labor force fell ill. Additionally, sick farmers meant unharvested fields and untended animals, piling on the losses.
Though little economic data exists for states and localities for this time period, the economic losses surely echoed throughout the U.S. and around the globe.
One 2020 study found that nations typically experienced a flu-related decline in GDP near 6% from 1918-1920. There is some evidence that wages increased in the U.S. as a result of the pandemic, as the illnesses and deaths reduced the labor supply for manufacturers across the country.
With fewer employees working with existing equipment to maintain or even increase production, economic theory would suggest that productivity per worker would increase and drive income growth. Indeed, research has found that the 1918 pandemic was linked to subsequent state-level income growth. Importantly, even though there is some evidence of gains, these gains must be placed in context of the large overall loss of economic activity, not to mention the overwhelming personal losses during the pandemic.
While there were economic consequences of the 1918 pandemic, most were found to be short-lived. One study found, however, that some negative effects were long lasting, as people who were born in the wake of the pandemic went on to achieve poorer education and economic outcomes in their lives.
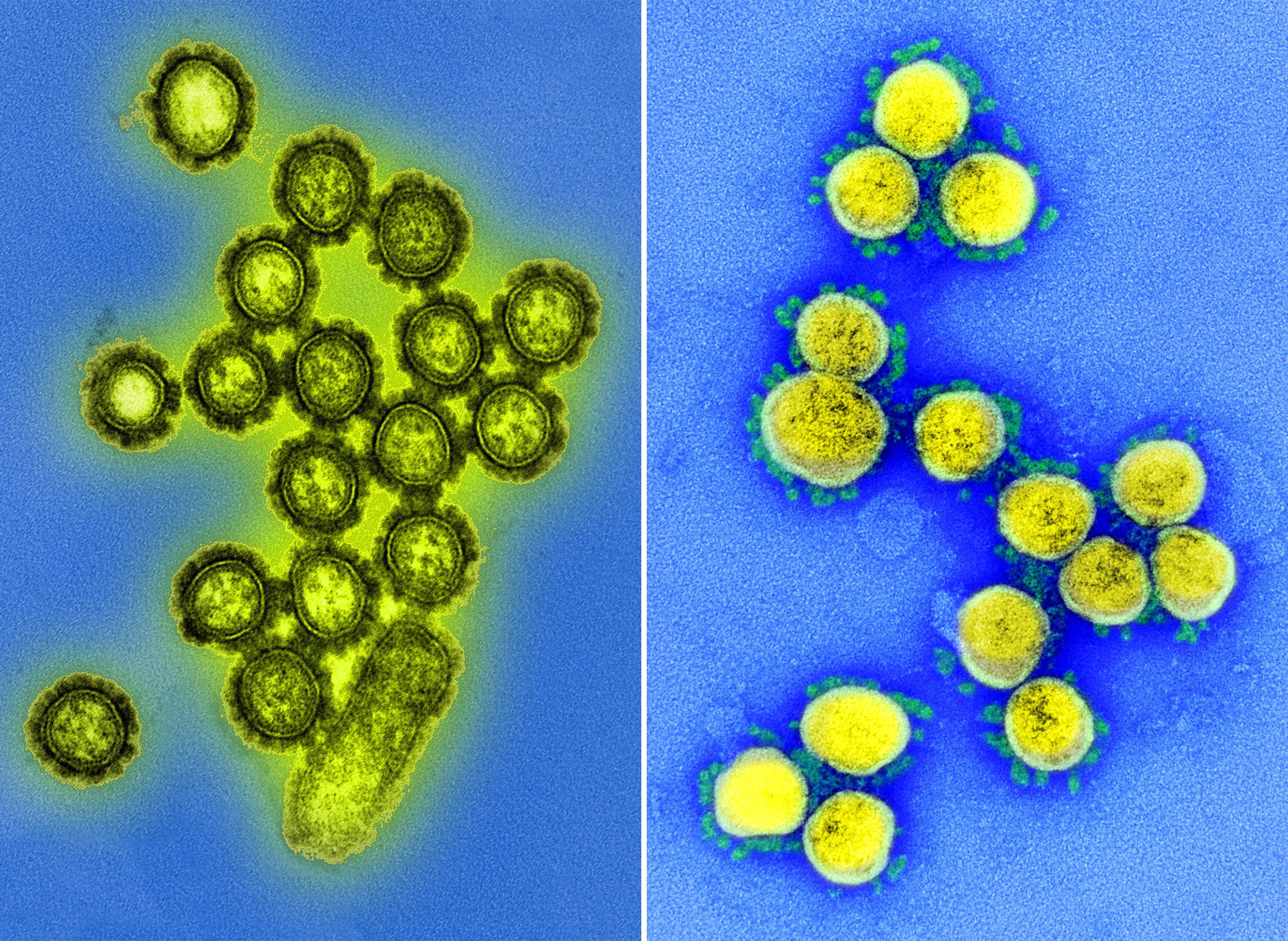
A comparison fraught with complications
Large differences between the economy and the nature of the viruses themselves make it difficult to compare the COVID-19 pandemic with the 1918 flu pandemic. For instance, transportation infrastructure has evolved dramatically. While the 1918 flu spread along highway and train routes, in 2020 humans can travel faster and over a much more extensive network. Supply chains and production methods are also much more geographically dispersed, making it difficult to isolate the effects of local outbreaks of COVID-19 as different regions encounter and address it.
The most vulnerable populations are different too. Those at greatest risk to COVID-19 are generally older and more likely to be out of the workforce, whereas the 1918 flu most severely impacted adults of prime working age, meaning the families of the sick likely lost a primary source of income. The economic effects of the 1918 pandemic could also be conflated with that of a war-time economy in the U.S., as World War I was just ending as the flu took hold.
In addition to these differences, in the 21st century, the U.S. and Wisconsin have a breadth of government policies and programs meant to address such economic challenges.
Wisconsin was the first state to enact unemployment insurance into law, but did not do so until 1932, meaning the stabilizing benefits of this program were not widely available during the 1918 pandemic. In 2020, between mid-March and mid-April, there were more than 400,000 new applications for unemployment insurance in Wisconsin. Similar to unemployment insurance, the Federal Old-Age, Survivor and Disability Insurance program — known as Social Security — only began taking shape as a program in the 1930s, so survivor and disability benefits that may have eased the economic burden for some families during the 1918 pandemic did not exist.
In 2020, the U.S. is more informed and more experienced at mitigating the effects of an economic downturn using fiscal and monetary policy. If, as anticipated, the nation finds itself in a recession, it would be the 19th downturn since the 1918 pandemic, including one that began in the late summer of that year.
In 1918, the Federal Reserve Bank, which administers monetary policy in the U.S., was only five years old and had mainly focused on financing the war effort. Even if the Federal Reserve had the tools and presence to act otherwise, prior to the 1930s classical economic thinking would have instructed policymakers to allow markets to correct themselves rather than intervene. With this history in mind, there was likely little impetus for a national economic response to the 1918 pandemic.
A vastly different policy approach
In 2020, there is a menu of policy options meant to ease the hardship of a declining economy during the COVID-19 pandemic, several of which have already been deployed.
Monetary policy, enacted at the discretion of the Federal Reserve, is often used to mitigate the effects of an economic downturn, mainly by lowering interest rates for debt incurred by large purchases such as homes and cars. These policies are meant to spur demand with increased consumer spending. The Federal Reserve has already lowered the interest rate to nearly zero and signaled an intention to keep it low for the near future. Furthermore, the Federal Reserve has initiated a strategy similar to the quantitative easing used during the Great Recession, alongside a suite of practices designed to stabilize suddenly volatile markets.
Meanwhile, Congress and the White House typically pursue fiscal policies centered on changing tax rates and government spending to ease the effects of a slowing economy. By mid-April, there were already three rounds of such policies enacted into law in response to COVID-19. The first initiative, in early March, committed roughly $8 billion in emergency funding to support the coronavirus response. The second initiative, known as the Families First Coronavirus Act, is expected to cost close to $200 billion. The third, enacted on March 27 and known as the Coronavirus Aid, Relief, and Economic Security Act, or CARES Act, centered on a $2.3 trillion fiscal stimulus package — the largest ever in U.S. history.
While many of these tools are familiar, the specific context of the COVID-19 pandemic is less so. Economic downturns are commonly initiated by one of three types of shocks: a financial shock, a shock to supply or a shock to demand. The COVID-19 pandemic includes aspects of all three, making the appropriate policy response especially complex and uncertain.
Still, these policies, though widely debated, put the country in a very different and, policymakers hope, better position than in 1918. If these measures work as intended, they would mitigate the downturn, aid a speedy recovery and, at the least, guarantee another important lesson in economic policy.
Tessa Conroy is an economic development specialist at the University of Wisconsin-Madison Division of Extension’s Center for Community and Economic Development and an assistant professor in the UW-Madison Department of Applied & Agricultural Economics.
This report was produced in a partnership between Wisconsin Public Radio, PBS Wisconsin and the University of Wisconsin Cooperative Extension. @ Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.