With storms, there are forecasts to rely on to help the community prepare. But health officials have few clues as to how the new coronavirus, COVID-19, will play out.
They’re relying on experience and close monitoring of the outbreak, which has killed 11 in the United States and sickened more than 120, but killed thousands elsewhere across the globe.
The one confirmed case in Wisconsin was someone who returned to Dane County from China. They are out of isolation and are fully recovered, according to state health officials. Tests on another six individuals were still pending as of 2 p.m. Wednesday.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
Prepping for a potential pandemic will likely include several state agencies, especially those linked to large gatherings or close quarters, like the state departments of tourism and corrections.
At a state Capitol briefing Wednesday held by state health officials for lawmakers, state Rep. Michael Schraa, R-Oshkosh, said he has eight correctional facilities in his district, many of which have staffing shortages where between 15 and 30 percent of positions are vacant.
“If there is an outbreak, do you have any specific plan to man these facilities?” Schraa asked.
Health officials didn’t address the staffing issues specifically but said they’ve had conversations with corrections officials and those who run nursing homes, which are also having trouble finding and keeping workers.
“If there’s a community that has a correctional facility and we have COVID-19 spreading in the community, we have to be proactive in the same way that we are about skilled nursing facilities to make sure we have attention paid to exposing people, visitation rules or screening like we do in health systems,” said Dr. Ryan Westergaard with the Wisconsin Department of Health Services.
Hospitals are bracing for an outbreak.
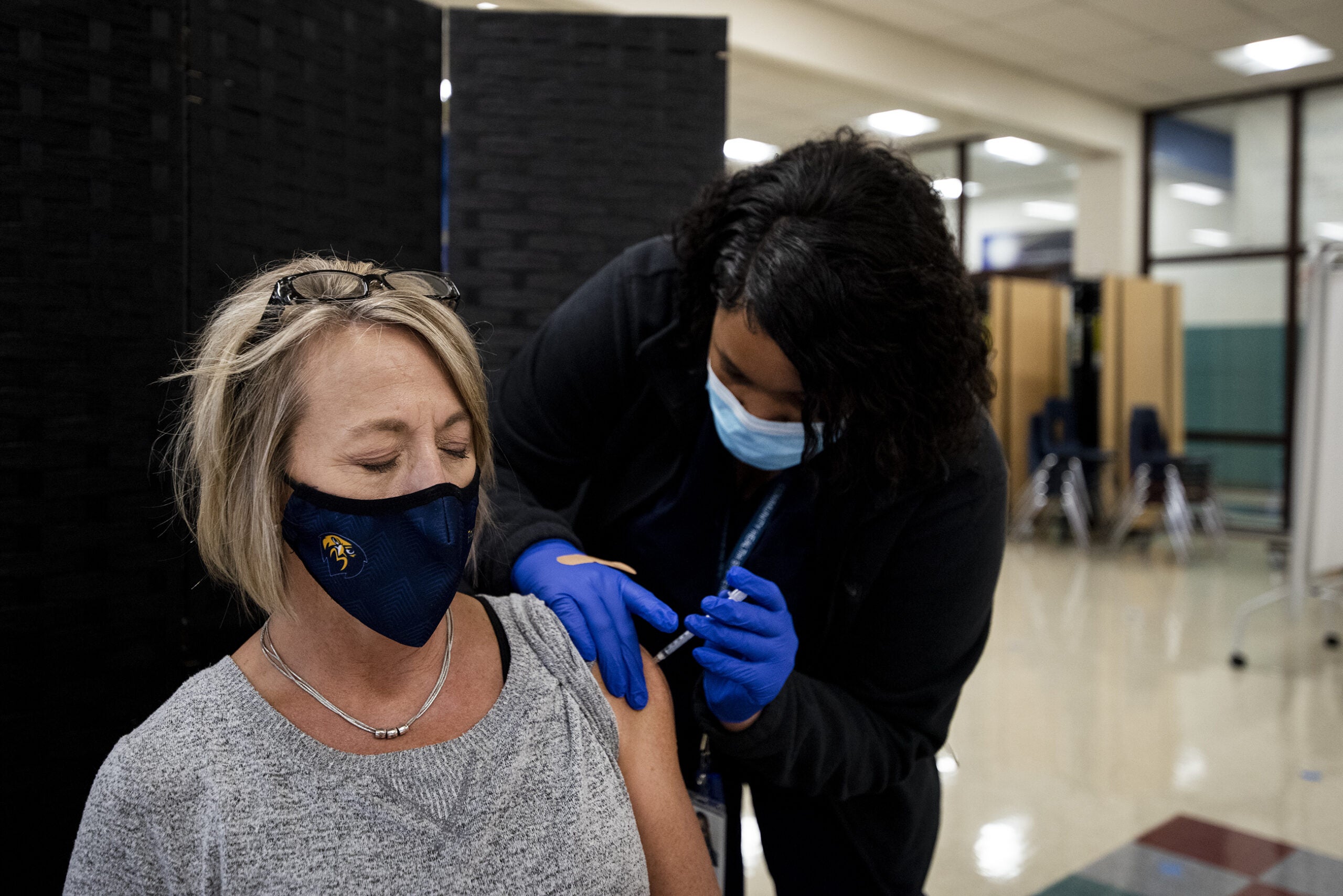
During a press conference at UW Hospital in Madison, doctors said they are making plans for increased testing and care of patients in addition to making sure there is enough personal protective equipment like N95 respirators, gowns, gloves and eyewear to safely deliver care to patients who are suspected or confirmed to have COVID-19.
“It seems community transmission will be inevitable. It’s already in the U.S.,” said Dr. Nasia Safdar, medical director for infection control and prevention at UW Health. The hospital is developing its plan for a surge of patients should the outbreak reach that level.
At this time, health officials say risk is low and remind everyone to wash hands frequently or use sanitizer not only to ward off COVID-19 but protect from a bad flu season that hasn’t peaked yet.
[[{“fid”:”1178966″,”view_mode”:”embed_portrait”,”fields”:{“alt”:”Nasia Safdar”,”title”:”Nasia Safdar”,”class”:”media-element file-embed-portrait media-wysiwyg-align-right”,”data-delta”:”2″,”format”:”embed_portrait”,”alignment”:”right”,”field_image_caption[und][0][value]”:”%3Cp%3EDr.%20Nasia%20Safdar%20holds%20an%20N95%20respirator%20mask.%20During%20a%20Wednesday%2C%20March%204%2C%202020%20press%20conference%20at%20University%20Hospital%20in%20Madison%2C%20she%20said%20the%20hospital%20is%20taking%20steps%20to%20conserve%20their%20supply%2C%20such%20as%20having%20medical%20providers%20reused%20masks%20and%20allocating%20one%20mask%20per%20patient%20with%20symptoms.%26nbsp%3B%3C%2Fp%3E%0A”,”field_image_caption[und][0][format]”:”full_html”,”field_file_image_alt_text[und][0][value]”:”Nasia Safdar”,”field_file_image_title_text[und][0][value]”:”Nasia Safdar”},”type”:”media”,”field_deltas”:{“2”:{“alt”:”Nasia Safdar”,”title”:”Nasia Safdar”,”class”:”media-element file-embed-portrait media-wysiwyg-align-right”,”data-delta”:”2″,”format”:”embed_portrait”,”alignment”:”right”,”field_image_caption[und][0][value]”:”%3Cp%3EDr.%20Nasia%20Safdar%20holds%20an%20N95%20respirator%20mask.%20During%20a%20Wednesday%2C%20March%204%2C%202020%20press%20conference%20at%20University%20Hospital%20in%20Madison%2C%20she%20said%20the%20hospital%20is%20taking%20steps%20to%20conserve%20their%20supply%2C%20such%20as%20having%20medical%20providers%20reused%20masks%20and%20allocating%20one%20mask%20per%20patient%20with%20symptoms.%26nbsp%3B%3C%2Fp%3E%0A”,”field_image_caption[und][0][format]”:”full_html”,”field_file_image_alt_text[und][0][value]”:”Nasia Safdar”,”field_file_image_title_text[und][0][value]”:”Nasia Safdar”}},”link_text”:false,”attributes”:{“alt”:”Nasia Safdar”,”title”:”Nasia Safdar”,”class”:”media-element file-embed-portrait media-wysiwyg-align-right”,”data-delta”:”2″}}]]Hospitals across the country are competing with consumers for face masks even though experts say healthy individuals do not need to wear them.
At Tufts Medical Center in Boston, there have been thefts of respirator masks and other essential protective equipment in lobbies and other high-traffic areas.
There haven’t been any thefts of masks at UW Hospital, but officials are trying to maintain their supply.
“It certainly is true that masks have been flying off (store) shelves,” Safdar said. “I think it’s a natural reaction when people are worried about something in the community that might be transmissible. Our approach has been to use signage and more monitoring of those kiosks where we have masks just to make sure they’ve being conserved for the people who really need them.”
The hospital is trying to conserve masks by having providers reuse them and allowing one mask per patient.
UW Hospital has set up a hotline people can call to learn more about COVID-19. That number is 608-720-5300.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.