For the first time mental health care providers are able to use telemedicine to treat their patients.
The federal government removed Medicare restrictions and temporarily relaxed HIPPA obligations during the new coronavirus pandemic, giving doctors nationwide a new opportunity to treat home-bound patients.
Being able to treat patients with mental health issues using Zoom, Skype or FaceTime could also present a future opportunity to address the mental health care shortage.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
“We don’t have enough psychologists, period,” said W. Hobart Davies, chair of psychology at the University of Wisconsin-Milwaukee. “It’s important that some of the rules have been relaxed during the pandemic, that really didn’t have any justification in protecting patients, will continue to see some reform.”
In Wisconsin, rural communities often have the hardest time providing mental health care. A 2018 report from the Wisconsin Policy Forum found 55 of 72 Wisconsin counties face a “significant shortage” of psychiatrists and 20 have no practicing psychiatrists at all.
“Exacerbating this problem is the fact the state’s psychiatrist workforce is aging rapidly,” the report found. “The average Wisconsin psychiatrist is 50 years old and 15 percent of the state’s psychiatrists are 65 or older.”
Before the temporary telemedicine coverage expansion was announced by the Centers for Medicare & Medicaid Services last month, patients who needed a telephone-based sessions with their physician had to pay out-of-pocket. Now, providers are being reimbursed by both public and private insurance.
Davies said most patients have been willing to make the shift to telehealth because they know it’s the only option during the state’s stay-at-home order, but there are some drawbacks.
“The people having the most difficulty are those having to arrange a private location in their house or apartment,” Davies said. “Some people have not told family members or roommates they are in therapy.”
But Davies said for a lot of patients, being able to speak to their doctor using telemedicine is a lot more convenient, since they don’t have to drive to an office during business hours.
“I’m hoping this will lead to reform and careful thought about what’s really in people’s best interest,” Davis thought. “I think it’s really interesting to see what clients prefer this and ask (if) they will be able to continue their sessions this way even after the pandemic.”
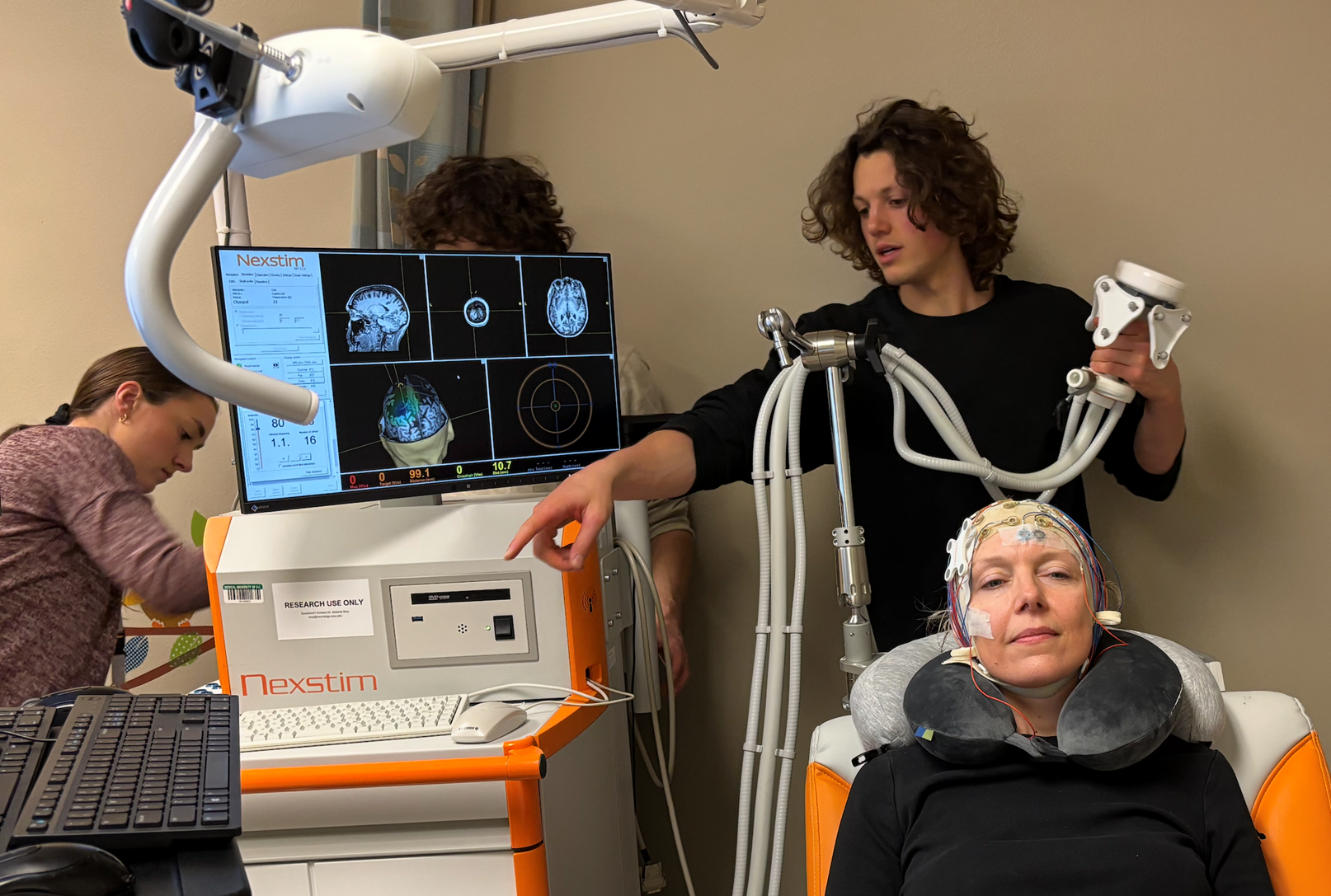
About 800 patients receive virtual care daily at Rogers Behavioral Health. Rogers is based in Oconomowoc with locations in Appleton, Brown Deer, Kenosha, Madison and West Allis. There are also clinics in California, Florida, Georgia, Illinois, Minnesota, Tennessee and Pennsylvania.
Rogers has been providing telepsychology for about seven years, but when the COVID-19 pandemic hit, the 17 outpatient clinics located across Wisconsin and in seven other states were converted to telehealth for outpatient counseling.
This all happened in less than two weeks, said Scott Johnson, chief operating officer for most of Rogers outpatient clinics, who has been leading the telehealth initiative.
Treatment ranges from alcohol and drug addiction to eating disorders to anxiety and OCD, said Dr. Stephanie Eken, medical director of outpatient care at Rogers.
“I think what all of our clinicians recognize is mental health issues, at a time like this, it’s such a stressor, all of our symptoms can increase,” Eken said.
Johnson said the public health emergency has led to innovations on how to serve patients.
“One of the populations that have been underserved historically are those who are not close to a Rogers clinic, especially in regard to a specialty service,” Johnson said. “I do see telehealth as a way to overcome the accessibility issue around distance or transportation to so many children, or adolescences or even adults who are too far away to have this to be an option, day in and day out.”
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.