Renae moves hedge clippers, gloves and used coffee mugs off a table in her backyard and wipes it down. She scans the lawn behind her modest home in the rural South for folding chairs and pulls up three. There are paper plates for pizza. Renae is about to host a gathering with a singular goal: saving lives.
“Hey baby, you sit right here,” Renae says to Christina, the first guest to arrive. “Just get your stuff ready.”
Stay informed on the latest news
Sign up for WPR’s email newsletter.
Christina opens a Mountain Dew and arranges her supplies: a new syringe, a lighter, a tiny metal cup and a baggie with brownish powder clumped in one corner. A test strip will confirm it includes fentanyl, the opioid that’s driving overdose deaths in the United States to record highs — an estimated 112,000 lives lost in the latest 12-month period.
Christina will use the powder anyway to appease her addiction and numb the pain of abuse, lost children and despair. On fentanyl, Christina gets temporary relief from three mental health diagnoses she struggles to manage: depression, anxiety and bipolar disorder.
Renae occasionally monitors illegal drug use at her home for Christina and a few dozen other people she’s grown close to over the years. It’s an informal, rarely discussed version of the controversial overdose prevention centers, also known as supervised consumption sites, where trained staff supervise people using drugs. Those clinics are endorsed by the American Medical Association and other leading medical groups but condemned by critics who say they sanction, even endorse, drug use.
Renae bustles around, looking for her glasses, pulling back her hair and chatting with a few other guests who have now arrived. But Christina’s in a hurry. It’s been nine hours since her last shot of an opioid. She’s anxious and has that feeling she’s going to be sick — the early signs of withdrawal.
Still, Christina has taken the time to come to Renae’s backyard because she trusts Renae to keep her alive.
Much of what happens next may be illegal, so this story will not include full names, locations or detailed timelines.
Renae, who has medical training, pulls up a stool next to Christina. She watches as Christina pours the powder into the aluminum cup, melts the contents with her lighter and draws the liquid into a syringe. The injection is over in seconds.
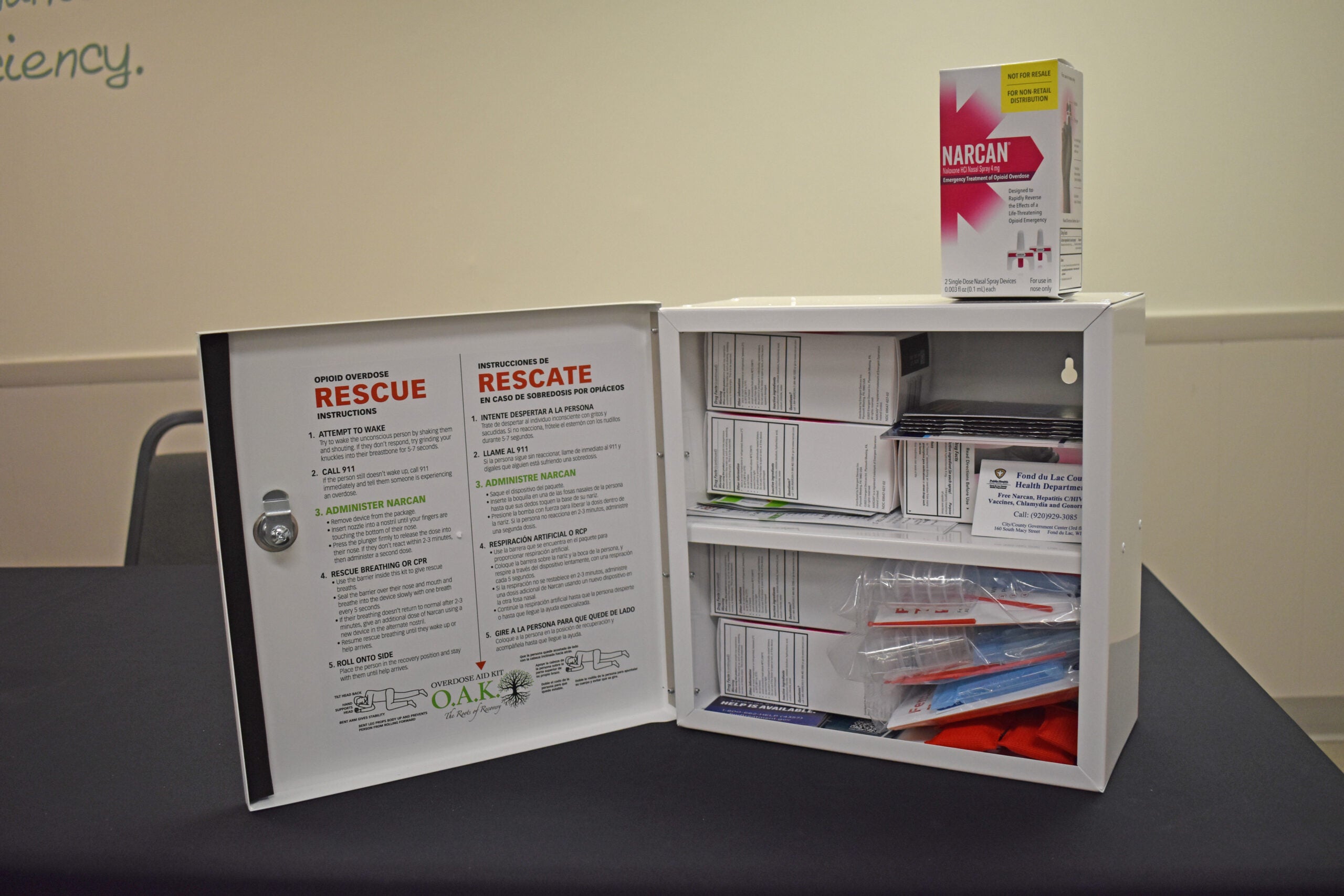
After the shot, Renae chats with Christina about whether she’s drinking enough water on this warm day. She turns a fan on Christina to help cool her down. Renae has Narcan handy, a brand of naloxone, the drug that can reverse an overdose. But this time, she doesn’t need it. About five minutes later, Christina stands up.
“I’m OK,” Christina says, and Renae agrees. Christina did not take a fatal dose of fentanyl today. Christina says thanks, the two women hug, and Christina walks away.
“This is seriously all it takes to keep somebody alive,” Renae says, hands spread toward her home-based supervised consumption site. “People die of overdoses because they’re by themselves.”
Nationwide, more than half of people found dead after an overdose were alone. Renae is determined to make a dent in those numbers by intervening when people stop breathing and helping them start treatment for their addiction if they are ready. In the meantime, she makes people comfortable if they nod off, checks vital signs and provides rescue breathing or Narcan when needed.
Renae is cautious about who she lets into her home, and there are rules. Call or text before you come. Only one person uses at a time. No drugs left behind. By Renae’s tally, she’s reversed at least 30 overdoses in the past few years. She’s never had to call 911. She’s never lost anyone.
What Renae sees as a life-saving mission is likely a violation of a federal law passed in 1986, during a surge in crack cocaine use. It says allowing illegal drug use in any designated space is against the law. At least one U.S. city and a few states are testing this law and have opened or plan to open supervised consumption clinics. It’s unclear whether federal agents will move to shut them down.
Opponents argue that Renae and others should focus on sending people with an addiction to treatment, not enabling their use.
“Yes, I enable, I absolutely do.” she says. “I enable them to leave of their own volition and not on an ambulance gurney or in a body bag.”
Many Americans condemn what Renae does. She understands why. Some years ago, when Renae’s daughter began using drugs, Renae would have condemned her own behavior too.
Keeping Brooke alive
Renae’s transformation from anxious mom to intrepid overdose prevention advocate started in her daughter’s early teens with lots of mother-daughter fights. Brooke would break a rule. Renae would respond like many parents do. She would ground Brooke and take away her cell phone. As she puts it, “I was wanting to force her to do what I wanted her to do.”
Renae says her approach “bombed.” She pushed and punished, and lost Brooke’s trust. Brooke says her mom’s demands — go to school, get a job, do the “right” things — were reasonable. But Brooke didn’t want to or didn’t feel like she could.
“I got tired,” Brooke says. “I didn’t want to let her down, so I just left.”
Brooke moved out at age 16. By 18, she was using opioids regularly. Renae often didn’t know where she was or whether she was alive or dead. Her despair is familiar to many parents of children with an addiction.
Renae imagined spotting Brooke somewhere, swooping her into a big bag and racing home, like scenes from a Bugs Bunny cartoon.
Then one day, after a month of unanswered texts and calls, Renae saw her daughter walking down a street, and something inside Renae flipped. All the fights, fury and disappointment melted into “pure joy.” Brooke was alive.
“That’s all that counts,” Renae remembers saying to herself. Her baby was still breathing.
Brooke didn’t want to talk and wouldn’t come home. Renae watched her go. But for Renae, everything had changed. She would give up on trying to control Brooke’s life. She would figure out how to keep Brooke alive instead.
A gut-wrenching dilemma
Renae’s new mission started with a simple step: She stocked up on Narcan for Brooke. It was a way back into her daughter’s life.
During each delivery, Renae did a quick scan. Brooke seemed reasonably healthy, and not too thin, but open wounds on her arms were getting worse. Renae could imagine why: Needles get dull with repeated use. Searching for a vein with a blunt needle creates bruising and wounds. And Renae assumed Brooke was sharing needles with friends who could have hepatitis C, HIV and other viruses. Transmissions are common among people without access to clean needles.
Renae knew clean needles could improve her daughter’s health. She also knew a needle she dropped off might deliver her daughter’s final shot of opioids, the one that would slow her breathing to a stop, turn her lips blue and end her life.
What was the lesser of two evils? Would Renae be encouraging, even sanctioning, Brooke’s drug use by giving her needles, or helping prevent injury and disease? Was she using needles as a way to see her daughter more often?
“The swirl of emotions was just insane,” Renae says. “The guilt, the anxiety, the fear.”
Renae ruminated for weeks. “It f****** spun like a record.”
In the end, the public health messages, and Renae’s need to see Brooke, won out. She placed an order online.
When the syringes arrived, Renae drove to the trailer park where Brooke was staying and handed her daughter the box. Brooke doesn’t have a clear memory of this moment that was so fraught for her mother. Renae remembers Brooke looking surprised, thankful and a little ashamed. Renae didn’t stay long. But she found she was too sick to drive. The debate kept pounding in her head.
“What did you just do?” Renae says she asked herself, again and again. “My nerves were shot.”
But in the weeks that followed, Brooke’s bruises disappeared and her wounds healed. Renae ordered more needles.
Possession of drug paraphernalia is a crime in many states. Renae didn’t know if what she was doing was allowed. She decided she’d ask for forgiveness if she got caught.
Renae’s effort would eventually become a registered syringe services program — a public health project to provide clean needles, medical care and referrals to treatment for people who use drugs.
Renae began adding items to her order, like alcohol pads and wipes, and increasing the quantities. Brooke kept giving away her needles and Narcan. Renae realized that trying to keep Brooke alive would mean supplying a whole bunch of other people, as well.
Renae was desperate to know the people her daughter shared food, shelter, drugs and Narcan with. Renae was counting on them to watch out for Brooke and save her daughter’s life if needed. But Brooke was keeping her friends away from Renae. So Renae found a way to introduce herself.
Hot dogs, soda and chaos
On a sweaty summer afternoon, Renae filled one cooler with ice, beer, bottles of water and soda. She used another to keep hot dogs and burgers from a local place warm.
Renae drove to the edge of a vacant lot between some cheap hotels and tents, the area of town where Brooke was living. It’s a predominantly Black neighborhood. Renae and her family are white. She pulled out a few lawn chairs, opened her trunk with the coolers, blasted her ’80s rock playlist and lounged back with a can and dog.
Renae’s rationale: “Everybody likes to eat, and hell, everybody’s nosy.”
Renae returned for several Saturdays, same drill. Eventually, people emptied her coolers and began to talk. Renae learned about another world of drug use. The people stopping for a burger and soda weren’t injecting opioids. They were using “bowls,” or glass pipes, to smoke methamphetamine. Some passed around glass tubes called “stems” or “roses” for smoking crack, or straws for snorting cocaine.
Renae suspected this meant sharing diseases, as well. She made lists of new items to order. And she kept handing out Narcan because fentanyl was showing up in meth and coke — killing unsuspecting people.
At home, Renae searched for the best deals on supplies for people who use stimulants. More boxes arrived. Her credit cards were almost maxed out. And she was, too. Lots of people had her cell phone number. They’d call in the middle of Renae’s work day or the middle of the night demanding needles, Narcan or some other kind of help.
“People expected I would drop what I was doing and go,” Renae says. “They’d say, ‘If you don’t come immediately then I’m going to die.’ I played into that for a while. Then I realized it wasn’t sustainable.”
That’s when Renae opened her laptop and discovered a national network of current and former drug users, their allies and families doing many of the same things she was doing. The work had a name: harm reduction.
Organizing to show love
Renae’s search connected her to groups offering free or discounted Narcan, needles and pipes. She made some new “besties” — veterans of the work she’d stumbled into. They helped her figure out how to run a program delivering care and supplies to hundreds of people who use drugs in her city — and try not to lose her mind.
Today Renae has a small team of volunteers. They set up in parks and vacant lots, where people move down a buffet line of crates and buckets. They fill plastic bags with drug supplies, condoms, dental dams, tampons, diapers and sometimes toothbrushes that a local church collects and donates.
Some people come just to say hi and get — or give — a hug. Renae’s face lights up.
“The stuff is just the carrot I dangle before the horse so I can make a connection,” Renae says. “I want my community to know what it feels like to be really loved so they never settle for anything less.”
Renae scans arms and legs for wounds that need care. She gets updates on medical appointments, arrest warrants and rehab wait times. If Renae runs out of supplies or has to change locations, she sends an alert online.
Local police haven’t blocked her outreach efforts. The county where she lives has seen an increase in overdose deaths since just before the pandemic, in line with a national rise, according to the Centers for Disease Control and Prevention.
She still makes some on-demand deliveries, but very few.
“We’re doing it right,” she says.
But programs like the one Renae runs are illegal in parts of the country. Opponents say handing out needles enables drug use, addiction and death.
Brooke worries about her mom. Renae works in neighborhoods where gangs are active and people may be desperate for money. And Brooke says her mom “takes s*** she don’t deserve.”
Like the time a woman confronted Renae, saying Renae gave the woman’s son a needle he used in what turned out to be a fatal overdose.
“Survivors’ guilt is real,” Renae says. “And it broke my heart because he was dead. But I would still give him the needle because it might have saved his life too.”
About 200 people stop by the parks and vacant lots where Renae distributes needles and other supplies every week. She spends about a quarter of her income, or more than $1,200 a month. Renae doesn’t like paperwork, but she might apply for nonprofit status to get a break on taxes. This would also make it easier to seek grants and accept donations.
These days, Renae laughs at the mama who drove around thinking she could scoop up her daughter and force her to stop using drugs. It’s one version of tough love — an approach many parents, addiction counselors and former people who’ve used drugs say works. For Renae, “tough love was torture.” But endless compassion, she says, can be pretty damn hard, too.
Inviting Brooke to use in the breakfast nook
Brooke would come home every now and then, in between her periods of sobriety, including four trips to rehab. Research suggests it can take people with a severe addiction four to five attempts at treatment over eight years on average before they achieve one year without drug use.
One afternoon about three years ago, Renae was in the kitchen when Brooke shuffled past her toward the bathroom. Renae could tell Brooke was in withdrawal and planning to use.
Many family members tell stories of trailing a child, spouse or parent to a bathroom or bedroom and listening — ear pressed to the door — for signs of life. Some were lucky to have naloxone with them. Others didn’t get into the room until it was too late. Renae didn’t want that to happen to Brooke.
“Why don’t you just sit down in here,” Renae remembers saying to Brooke. “It’s OK, I won’t watch.”
Brooke hesitated. She wanted to use alone, but Renae would know what to do if Brooke needed help. Brooke went back to the table.
“It was weird though,” Brooke says. “I ain’t going to lie, it was weird.”
Renae turned to face the kitchen sink. In a few minutes, when she heard whimpering, Renae looked back. Brooke had poked herself many times in her unsteady state. Renae saw blood on the floor.
“At that moment, I didn’t feel like her mama,” Renae says. “She was a patient. She needed help.”
Renae wiped the blood off her daughter’s arms and helped her calm down. Then, Renae did something else she’d never done before. She sat with Brooke for the shot, and stayed by Brooke’s side until Renae was sure Brooke was not going to overdose. For this decision, Renae says, there was no time for internal debates.
“It’s just what I knew had to happen,” she says.
The afternoon cemented an unusual mother-daughter bond.
“For her to have the heart to do that for me?” Brooke says and then pauses. “I can’t promise I could do that for my child. That takes some strong will.”
Years later, Renae continues standing watch, without judgment, for people using drugs.
In Renae’s kitchen or backyard, people won’t be robbed or raped while they are too sedated to fight off an attacker. They don’t have to worry about heat stroke, drenching rain or cold nights.
If a guest nods off, Renae lets them sleep, on their side in case they throw up. If the person needs oxygen, Renae starts rescue breathing. She uses Narcan when breathing assistance isn’t enough.
To Renae’s way of thinking, the country already has supervised consumption sites. They’re called bars. There are significant differences, but Renae is making a point heard often among people who use drugs. Addiction is the same disease — but alcohol is legal, while many other drugs are not.
There’s no database of people like Renae — parents, friends and outreach workers who monitor drug use for people they care about. Those who have done it say it happens quietly, with little guidance and some shame, in bedrooms, cars and alleys.
“What I’m doing is not unusual. No, no, no,” Renae says. “My willingness to talk about it? Now, that’s a different story.”
If there’s a line Renae is not willing to cross to keep her loved ones alive, “I ain’t found it yet,” she says.
Helping clients start treatment, even when that, too, may be illegal
Late in the afternoon, when Renae’s backyard-based overdose prevention effort is wrapping up, a woman Renae’s known for years comes by. Renae would be happy to monitor her use, but the woman says she just needs some needles and Narcan. A. tells Renae she’s struggling to wean herself off fentanyl, and is only using enough of the powerful opioid to avoid withdrawal.
“But it’s scary,” A. says. “If you’re doing it, you’re putting yourself at risk. And I’m fully aware of that every time.”
NPR/WBUR agreed to use A.’s first initial because she has a distinctive name.
A. recently tried to stop using fentanyl altogether and start treatment with Suboxone, a brand of the addiction medicine buprenorphine. But A. says a local treatment program required a 72-hour wait between her last shot of fentanyl and the first dose of Suboxone. It’s a rule addiction specialists say is outdated. A. couldn’t make it.
“I tried, but the withdrawal was so bad I wanted to kill myself,” A. tells Renae. “People say, ‘Just get sick and get it over with,’ but I can’t.”
Renae listens, her hand on A.’s knee, as A. starts to cry. Then, here in her backyard, Renae offers another service aimed at keeping A. alive, one that also comes with legal risks. Renae shifts from monitoring drug use to offering treatment.
“When you’re ready, I got you,” Renae tells A., and explains her plan.
It’s a technique called microdosing that is increasingly being used at many medical centers. A. would take tiny doses of Suboxone while she’s tapering off fentanyl, which can ease the transition to the new drug. Renae isn’t licensed to prescribe Suboxone, but either she or A. will find a way to get some. Renae says a half-dozen people she coached through microdosing Suboxone are still on it, and not fentanyl, two years later.
A. weighs Renae’s offer. She isn’t ready for another painful withdrawal, but with Renae’s guidance, she’s “close, really close.”
“It does give me hope that she hasn’t given up on me,” A. says. “It’s just hard to believe I’m worth that.”
For Renae, this is the core of her work — relieving shame and helping restore dignity.
A. says lots of people are willing to help her as long as she does “this or that.” With Renae, A. says, there are no expectations or judgment, just kindness and compassion.
“If there was more of that,” A. says, “I can’t imagine how different things could be.”
No end in sight, but Brooke is alive
When A. leaves, Renae reviews the week ahead. She may have to cancel deliveries. An agency that was supposed to send needles isn’t coming through, and she’s out of money.
There are many weeks when Renae learns someone she knows has died after an overdose. Some days, it’s hard to get out of bed. Seeing Brooke lifts Renae’s spirits.
Brooke is no longer using opioids but says she smokes weed and takes other drugs recreationally. The mother and daughter still annoy each other sometimes, but they’re repairing their relationship.
“Not everyone’s got a mama like my mama,” Brooke says with a laugh.
Renae used to think her goal was to keep her work going as long as Brooke needed help. But now Renae can’t imagine stopping.
“I never intended to have this life. I thought I’d give her some Narcan to keep her alive, she’d go to rehab and everything would be OK,” Renae says. “Now, I can’t turn away. I’m in it forever — or as long as I last.”
9(MDAyMjQ1NTA4MDEyMjU5MTk3OTdlZmMzMQ004))
© Copyright 2025 by NPR. To see more, visit https://www.npr.org.9(MDAyMjQ1NTA4MDEyMjU5MTk3OTdlZmMzMQ004))