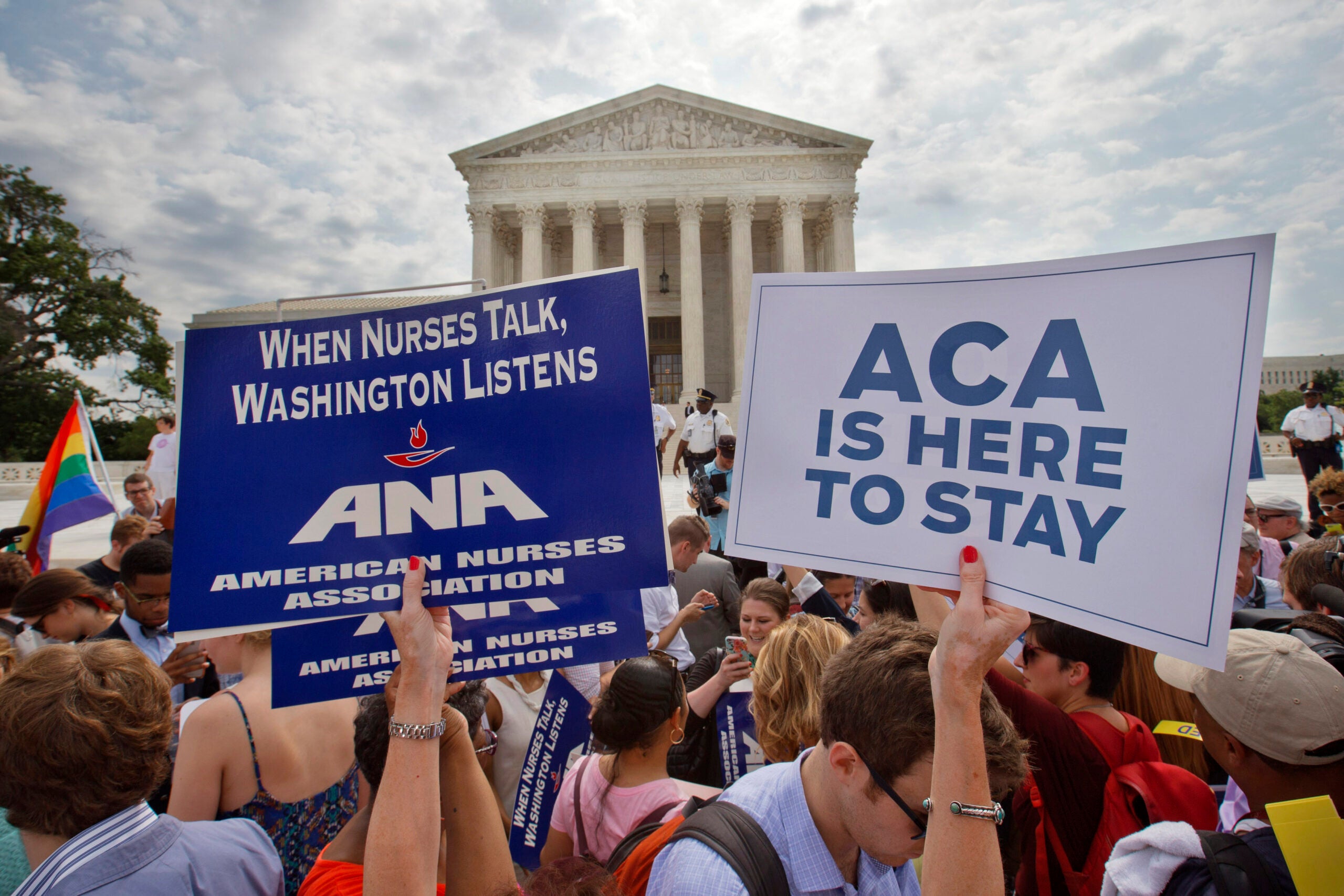
The Biden administration has implemented a new regulation that will prohibit medical debt from being factored into consumer credit reports.
Americans hold at least $220 billion in medical debt, and that debt disproportionately affects women, Black Americans, and Americans with disabilities. The agency that created the rule estimates that it would raise affected Americans’ credit scores by an average of 20 points.
But the rule is already facing a lawsuit from credit industry groups. And because federal rules don’t go into effect until 60 days after a rule is published, its fate will ultimately be determined by the Trump administration.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
WPR’s “Wisconsin Today” spoke about it with Bobby Peterson, executive director and public interest attorney for ABC for Health, a nonprofit law firm that advocates for healthcare access for children and families.
The following interview has been edited for clarity and brevity.
Lee Rayburn: Do we have an idea of the amount of medical debt that is in Wisconsin?
Bobby Peterson: Annually, the Wisconsin Hospital Association issues a report. This is only hospital-related debt, but it’s fairly significant. In this last year, 2023 . . . it was nearly $1.4 billion in unpaid medical bills. That includes charity care, but also bad debt. It’s been in that $1.2 to $1.4 billion range for the last several years.So it’s a big chunk of money. It affects a lot of people, and trying to sort out medical debt is really not for the faint of heart.
LR: Do you see a connection between medical debt and health outcomes?
BP: When we think about people that have large amounts of medical debt … we have to remember that oftentimes people are trying to deal with these complicated questions about coverage and eligibility while they’re dealing with an illness for themselves or a family member.
People will delay care or avoid care. The research is pretty strong out there that a lot of people will delay care if they have existing medical debt. It’s a situation where things can get worse and then get a lot worse, so when you end up going to the doctor, it might even be even more expensive.
LR: The proposal to remove this medical debt from credit reports is already facing a lawsuit from credit reporting industry groups. Do you see their side of the argument? They claim that the rule violates the Fair Credit Reporting Act and that it may impede their ability to do their work.
BP: I don’t see it that way. I look at it through the lens of the clients that we work with and the work that we do for a lot of populations that are facing challenges. When you’re trying to understand your coverages and services … There’s a lot to go through. And when you’re sick and trying to help a family member, trying to navigate this is nearly impossible.
I think taking medical debt out of the equation is going to help increase credit scores for people, help people get ahead and maybe identify financial opportunities moving forward. I don’t really see a real, legitimate reason for using medical debt as a part of the credit scoring process.
LR: There are some places where medical debt is not included in credit scores. What can we learn from them?
BP: I think generally we’re going to find that … if you take this out of the equation, people are going to have more opportunities to obtain credit, obtain apartments, obtain other services that they need. But once you throw medical debt in there, it really becomes this electronic debtors’ prison.
And it’s simply because you were sick, simply because you didn’t have the ability to identify all these different covered sources that might have been available. You know, your hospital may even have some responsibilities to provide financial assistance. Hospitals as nonprofits are required to provide a certain level of charity care to people out there, and oftentimes we have to dig into their rules and requirements to make sure that they’re providing that correctly and appropriately to people.