This story was originally published by Wisconsin Watch.
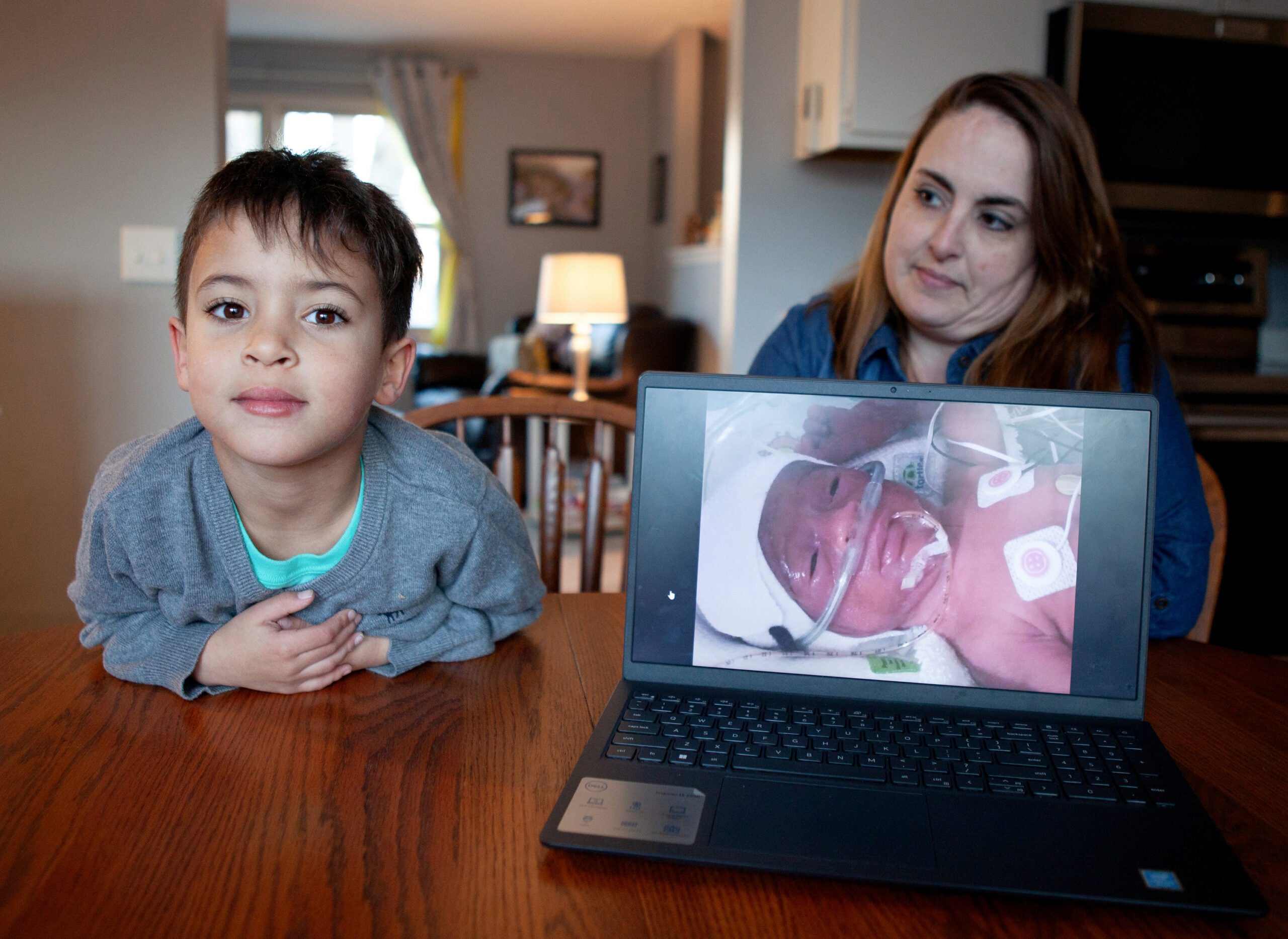
Emily Schmit didn’t expect to be a mother. She was told at a young age that she would likely be infertile, so when she took a positive pregnancy test in 2017 at age 30, she was overjoyed. She made plans to hold a baby shower, decorate a room and take maternity photos.
Those plans were cut short, however, when she went into labor at 28 weeks, giving birth to her son three days later. Born at just 2 pounds, 10 ounces, he spent his first 60 days in the neonatal intensive care unit.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
To complicate matters, Schmit had recently left her job, qualifying her for the state’s BadgerCare Plus Medicaid program. In Wisconsin, where 2 of every 5 mothers give birth on the program, coverage stops for most recipients at 60 days. For Schmit, that meant leaving the NICU also meant the end of any postpartum care for her.
“There was literally no support for me, and once he was born, that was it. They were just like, ‘OK, well, we don’t want to see you. We want to see the baby,’” said Schmit, of Mount Horeb. “Instead of me having the opportunity to say, ‘Hey, something’s not right,’ or, ‘I need support,’ I didn’t even have that option because of the Medicaid program.”
Each year, at least 25 Wisconsin women die during or within one year of pregnancy, with less than a third occurring during birth.
Experts said extending the coverage period for women insured under Medicaid could help new mothers with depression and other health issues and save lives among Wisconsin’s most vulnerable residents.
Yet the Legislature has turned down extensions with bipartisan support on multiple occasions. That includes a bipartisan bill that passed the Senate this session but the Assembly didn’t take up, making Wisconsin one of just four states without plans to implement a full-year extension.
Proponents: Extension would protect mothers’ health
Doctors said an extension would allow patients struggling with postpartum depression, anxiety, PTSD, schizophrenia, bipolar illness, substance use disorders and other mental health issues to continue therapy and medication amid sleep deprivation and stress.
“The year following a delivery is a very important year with huge life changes and where having adequate health care is absolutely essential,” said Dr. Lee Dresang, a family medicine doctor at UW Health and a professor at the University of Wisconsin School of Medicine and Public Health.
Of the patients he followed with postpartum depression, “exactly zero magically got better at 60 days after delivery,” he said during a legislative hearing.
Maternal mental health conditions are the most common complication of pregnancy and childbirth, according to the Maternal Mental Health Leadership Alliance, with suicide and overdose the top causes of death in the first year postpartum. Of the 1 in 5 women who struggle with maternal mental health conditions, 75 percent don’t receive treatment.
The emotions that manifest amid postpartum anxiety create a vulnerable time full of doubt and shame that can become overwhelming, explained Sarah Ornst Bloomquist, the co-founder of a Milwaukee-based perinatal mental health organization, Moms Mental Health Initiative. Thoughts might manifest in the form of, “If you really wanted to be a mother, you wouldn’t feel this way,” “You are not a good mom,” or “Your family will be better off without you.”
Bloomquist herself had lots of energy in the days leading up to the birth of her first child. But anxiety overcame her as soon as her son was born — a feeling that worsened during the postpartum period.
“It was a shock to my system every time they woke me up and brought him to me,” Bloomquist said. “It felt like I was just being zapped with this onslaught of anxiety and pressure with no way out, like I was just trapped.”
In the year after she gave birth, Bloomquist switched medications multiple times, met with postpartum specialists and sought out perinatal therapy, all of which was covered under her private insurance. She can’t imagine what her first 60 days postpartum would have been like without those resources, calling it “a nightmare” that would have set her up “for failure.”

Finding a therapist who understands those issues can take time. Amid stigma and a lack of resources, many women won’t reach out for help in the first place — and when they do, “one little deterrent will shut them down for good.”
While about 50 to 85 percent of women experience postpartum blues in the first few days to weeks after delivery, postpartum depression doesn’t usually emerge until two to three months postpartum, though it may occur earlier.
The second time Bloomquist gave birth in 2012, it wasn’t until two months postpartum that she started experiencing symptoms of depression.
“It’s very heartbreaking and it cuts you down to the core, this disease. It affects your entire perception of motherhood and what kind of mother you are and can be,” Bloomquist said. “These legislators … I don’t understand. It could happen to one of their children or grandchildren and most likely has.”
Women during pregnancy and in the postpartum period may also experience elevated weight and thyroid conditions, seizure disorders, high blood pressure disorders, diabetes in pregnancy and substance use disorders, among others, according to the CDC. Preexisting chronic conditions like hypertension, diabetes and heart disease may worsen during pregnancy or postpartum.
Lawmakers previously pushed for a 90-day coverage period. The 2021 state budget required DHS to request federal approval of a Medicaid plan to extend postpartum eligibility to 90 days, but the federal Centers for Medicare and Medicaid Services in January indicated to DHS that it doesn’t intend to approve a request for a new demonstration waiver for a coverage period shorter than 12 months.
Contraception is “particularly an issue” that would benefit from an extension beyond 60 days, according to Dresang. More time would allow doctors to recommend waiting on patient-centered care, including IUDs and other birth control.
During the pandemic, enhanced federal funding for state Medicaid programs through the Families First Coronavirus Response Act ensured that postpartum individuals covered by Medicaid had continuous coverage, but that coverage ended last April. Dresang said having the benefits clients experienced was a “really essential and wonderful silver lining.”
“I would hope that legislators could listen to the patients and health providers who witnessed how life-saving and helpful that extra coverage was to make it permanent and take advantage of this 12-month … extension while it’s available,” Dresang said.

Tina Elliott, a psychotherapist in Madison, first qualified for BadgerCare when her and her husband’s work hours dropped during the pandemic. She gave birth to her first child that April and has been on the program since, calling it “incredible” to have continuous coverage.
“With BadgerCare, you can go and get it covered and get it taken care of,” Elliott said. “If you have a marketplace plan, you probably have (such) a high deductible that you are always thinking, ‘Can I afford even the deductible because I’m already paying a premium? And how much is this going to affect my family to pay this bill?’”
Savannah Bertrand, of the Chippewa Valley area, gave birth to her daughter on Medicaid in February 2020. Continuous enrollment allowed her to seek services for hypertension and additional mood stabilizers for the postpartum depression she developed.
“I probably wouldn’t have even sought any help if I knew that the postpartum Medicaid wasn’t extending its limit,” Bertrand said.
Bertrand, who is now a Nurse-Family Partnership parent ambassador, said the economic output of investing in her mental health “was enormous” for her long-term postpartum success. The extension also allowed her family to expedite genetic testing, which led to an early autism diagnosis and enrollment in early childhood services by the time her daughter was two months old.
“Even if my daughter would have gotten on Medicaid, say a month later with backdating, that would have all been pushed off at least until the summer,” Bertrand said.
Currently, when a mother’s Medicaid eligibility is redetermined after 60 days, eligibility is reduced from 306 percent to 100 percent of the federal poverty level. Women whose income is above the federal poverty level, which is $1,703 per month in Wisconsin for a single mom with one child, must seek private marketplace coverage or lose insurance.
Mothers who lose Medicaid eligibility may experience churn, which refers to the period someone is uninsured when disenrolling and reenrolling in insurance programs due to different eligibility requirements. As a result, they may miss appointments and lose access to necessary treatment and medication, according to Amy Domeyer-Klenske, the chair of the Wisconsin section of the American College of Obstetricians and Gynecologists.
“You have to do all of this paperwork and applications when you’re not getting enough sleep, you may be suffering from a postpartum mood disorder, you’re experiencing really huge bodily changes and health stressors and you’re newly a parent,” Domeyer-Klenske said. “It’s this high-risk time for parents that we’re asking them to reapply and requalify for insurance.”
It’s sad to think they are not allowing abortions and forcing women to raise children and won’t even support women and babies for the first year of life.
Emily Schmit
Wisconsin an outlier
People with incomes up to 138 percent of the federal poverty level receive pregnancy-related Medicaid coverage for 60 days postpartum under federal law, after which states determine coverage. Wisconsin sets the income threshold at 306 percent during that 60-day period, which is the highest level of all 50 states.
Following the 2021 state budget requiring DHS’ waiver request, the Republican-run Legislature again rejected Gov. Tony Evers’ attempts to include an extension in the budget this year.
But Congress’ American Rescue Plan Act of 2021 and consolidated Appropriations Act of 2023 gave states a permanent option to receive federal matching funds for 12-month extensions. Forty-three states and Washington, D.C., have implemented a 12-month extension, and three are in the process. Wisconsin has not.
A bipartisan bill would put the state on a fast track there. Introduced in March, the bill would have extended Medical Assistance eligibility for postpartum care from 60 days to 12 months. The Senate passed the bill 32-1 on Sept. 14, but the Assembly never scheduled it for a floor session before adjourning for the rest of the session on Feb. 22. A previous version last session failed to get a floor vote in either chamber.
Assembly Speaker Robin Vos, R-Rochester, has pointed out Wisconsin’s high Medicaid income eligibility limit. Vos in a June 13 Wisconsin Health News event said he doesn’t support a Medicaid postpartum expansion, adding that “we give away too much free stuff.”
“When you make a choice to have a child, which I’m glad that people do, it’s not the taxpayers’ responsibility to pay for the delivery of that child, right? We do it for people who are in poverty,” he said. “But to now say beyond 60 days, we’re going to give you free coverage, no copayment, no deductible, until a year out, absolutely not.”
Schmit said it was “extremely disheartening and frustrating” that Vos blocked the bill.
“It’s sad to think they are not allowing abortions and forcing women to raise children and won’t even support women and babies for the first year of life,” Schmit said.

Advocates have expressed frustration over the state’s lack of urgency. Wisconsin’s waiver proposal sought the shortest extension at 90 days.
Wisconsin Republicans also have refused to expand Medicaid coverage with federal funding available for the past decade under the Affordable Care Act. States that expanded Medicaid were significantly associated with lower rates of maternal mortality compared with non-expansion states, according to a widely circulated February 2020 study.
Like many health issues, postpartum complications affect women of color at a disproportionate rate. In Wisconsin, Black women are five times more likely to die of pregnancy-related death than white women, according to DHS, compared with 2.6 times higher nationally.
Jamie Daw, an assistant professor at Columbia University Mailman School of Public Health, said the crisis is on policymakers’ minds in a way it hasn’t been historically. Comparing it to how awareness about infant mortality rose as an issue in the 1980s, she said maternal mortality is “having its moment.”
“Half of these pregnancy-related deaths are happening in the year after birth, which is a huge rethinking of the entire problem. When it comes to maternal mortality, the traditional focus has been on pregnancy and childbirth,” Daw said.

Continuous coverage has bipartisan support
In the wake of the Supreme Court ruling that overturned Roe v. Wade, legislation increasing postpartum coverage has generally been bipartisan. Testimonials in support of the standalone bill included Pro-Life Wisconsin and the Wisconsin Catholic Conference, as well as the American College of Obstetricians and Gynecologists and Kids Forward.
Sen. Joan Ballweg, R-Markesan, one of the lead authors of the bill, said she can’t think of any other issue with this much support from registered organizations.
“As a pro-life community, we think that this is an important piece to making sure that healthy moms make sure that babies are healthy,” Ballweg told Wisconsin Watch. “Science and health care have told us that we need to extend this coverage to make sure that we aren’t causing women to fall through the health care gaps.”
Schmit agreed that mothers and babies need to be thought of as one joint unit. She said a full-year extension would have helped her get back on her ADHD and anti-depression medications, which she couldn’t afford to pay for out of pocket. She also would have reached out to a postpartum therapist.
Since giving birth to her son, she’s advocated for an extension with the nonprofit maternal health group March of Dimes, speaking at their “Day of Action” at the state Capitol in November 2021 and serving as a group ambassador.
“There’s all this buzz when baby’s born and then you go home from the hospital. And that’s it. What do you do now?” Schmit said. “How am I supposed to continue to care for this little baby … if I myself am over here in the darkness feeling completely out of control and lost?”
Conservative states expand coverage
Daw noted that other states that historically have had lower Medicaid generosity like Missouri and West Virginia have implemented or are in the process of implementing a 12-month extension.
“Many states where there has been resistance against Medicaid expansions, like Tennessee or Texas, they’ve gone ahead and implemented the postpartum extension with very little fanfare,” Daw said. “Generally this has been kind of a bipartisan policy proposal, and it’s been accepted from red states and blue states, an unusual feat in the world of Medicaid policy.”
Schmit said she thinks the bill hasn’t moved forward because of a stigma associated with Medicaid recipients, and she noted that doctors and health care staff “instantly” treated her differently once she was switched onto the program. Schmit said her health concerns were often downplayed and that she was talked to condescendingly during her pregnancy.
“Regardless of your socioeconomic standing, you should still be able to be safe and secure,” she said.
The nonprofit Wisconsin Watch (www.WisconsinWatch.org) collaborates with Milwaukee Neighborhood News Service, WPR, PBS Wisconsin, other news media and the University of Wisconsin-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by Wisconsin Watch do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.