The fall is always one of the busier times of the year to be a school nurse.
Kids who haven’t been together in months begin sharing classrooms — meaning schools become a petri dish for cold and seasonal flu germs. At the same time, nurses are checking on kids’ vaccine compliance to make sure they got all their required shots before school. Like teachers, they’re also getting to know new students, especially those with chronic illnesses.
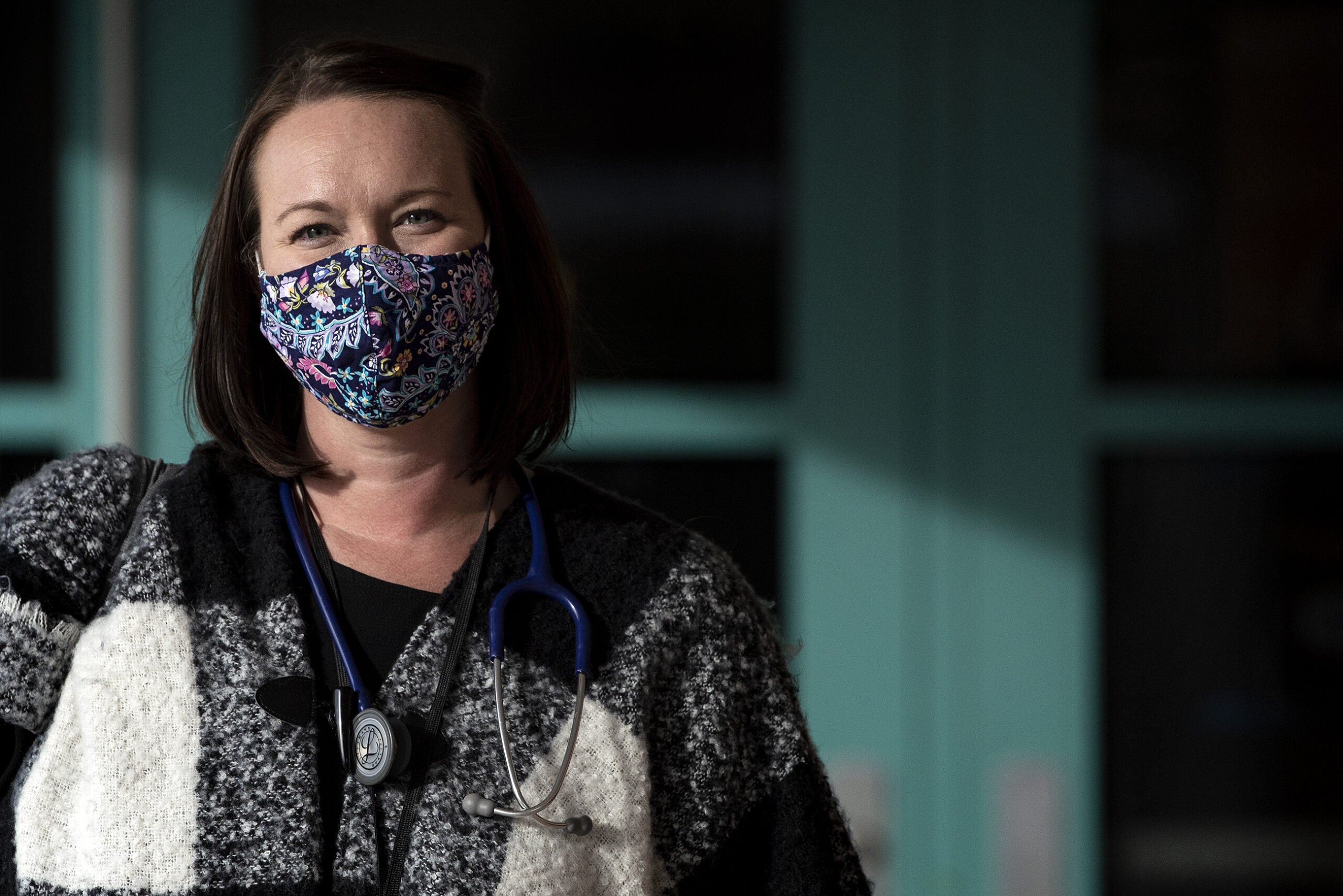
“I think the common misconception is that we’re just handing out Band-Aids, and that’s not the case,” said Brea Sanders, nurse for the Whitnall School District. “There’s a lot of case management, and a lot of supporting students to remain in school that have chronic health conditions.”
Stay informed on the latest news
Sign up for WPR’s email newsletter.
That’s, in part, what attracted Sanders to the job. She’s on her fourth year in school nursing, after previously working at Children’s Hospital in Milwaukee and Froedtert Hospital’s cancer center.
“I really liked the aspect of working with kids when they’re in the community, and kind of in their element,” she said. “I really work with a lot of kids who have chronic illnesses, and to see how they manage those conditions and still tackle their daily activities, it’s a really cool thing to see.”
Sanders is the only nurse in a Milwaukee County district of about 2,400 kids, though Whitnall also employs health aides in each school who help her stay on top of things.
As waves of budget cuts hit Wisconsin schools over the past decade, some cut hours for their school nurses, or eliminated the position entirely. Some grants and partnerships with local hospitals filled in a few gaps, but as of the 2019-2020 school year, employment records from the state Department of Public Instruction (DPI) showed only about 300 of Wisconsin’s 421 public school districts have nurses, many with student-nurse ratios similar to Sanders’ in Whitnall. Those that do have nurses have seen them step into a larger role this year, as districts rely more on medical experts to help them spot, trace and mitigate the spread of COVID-19.
Katie Johnson is a nurse and researcher at the University of Washington. She’s written about the role of school nurses in keeping kids in the classroom who might otherwise miss school due to chronic health conditions or other issues. She’s also tracked the prevalence of school nurses, and how many students they serve, around the country.
“It’s really quite stunning to think of being responsible for that many children, particularly vulnerable children who have health issues,” Johnson said. “Your practice looks very, very different when you have that many students, than a nurse who has a few hundred students.”
Sanders, who worked part-time for her first three years at Whitnall, added hours this year as her district school board anticipated bringing students back into buildings. She’s now handling much of the district’s contact tracing, notifying families who may have been exposed and narrowing down where the coronavirus might have spread.
In the Sun Prairie School District, nearly all students are learning virtually, though a few small groups of children who need more special education support have been going into school buildings for lessons. Still, the district’s two nurses say it’s the busiest fall they can remember.
“We still have to do things like immunization compliance, connecting with our students with chronic health conditions, making sure teachers are aware of the health needs of their students — even if they’re not in person in front of them,” said Elizabeth Feisthammel, known to students as “Nurse Elizabeth.”
She and her co-nurse, Debra Brown, are still having their usual conversations with teachers to alert them to, for example, a particular allergy, and to figure out a plan for administering emergency treatment — only this year it’s over the phone, instead of in person. Feisthammel said it’s still important for teachers to be aware of any conditions that may mean their students miss class more often even in a virtual environment, so teachers can figure out how to keep them up to speed.
Feisthammel and Brown have been preparing for COVID-19 since January, when initial reports out of China started raising concerns that the virus could become the kind of global pandemic that many disease experts have been anticipating for years. Brown vividly remembers a meeting with DPI’s nursing consultant in February, in which COVID-19 dominated the conversation.
“I remember talking with the nurse at DPI, and just that her gut was telling her it would be bad,” Brown said. “I think it was on the radar of school nurses pretty early on.“
When schools closed down, Brown and Feisthammel became a kind of clearinghouse for COVID-19 information.
“Guidance changes regularly, so keeping on top of that, to make sure we’re a resource for staff, students, administrators with the most up-to-date guidance coming out of the CDC, local public health, and state public health. That’s a big part of it,” said Feisthammel.
They’re also modeling disease-reduction behavior for students and staff, said Brown. The two nurses, who share an office, have been trying to minimize the time they’re both in the same room, and keeping a careful 6-foot-minimum distance, wearing masks and washing their hands when they do share a space.
COVID-19 may be a new challenge for school nurses, but it’s not unusual for their jobs to adapt to new concerns in the community.
Lauren Glass, head of the University of Wisconsin-Milwaukee’s Center for Nursing History, said she remembers vaccine clinics run by her school nurses growing up, where she’d get her necessary shots within the school building. Some early school nurses also handled more complex procedures — Glass pointed to a rather controversial project in 1906 when nurses and doctors were sent into public schools to remove students’ tonsils. Most of their work, though, focuses on less-invasive prevention and case management.
“School nurses have had an extremely important role over time … with the kids and (to) help the families access resources that they need for, particularly for children with disabilities,” Glass said.
Some think nurses’ roles may shift yet again as a result of COVID-19. Researchers and medical professionals still know relatively little about the long-term effects of COVID-19 on young people. If it does prompt chronic respiratory or circulatory issues later on, nurses like Sanders, Brown and Feisthammel will likely have to figure out how to monitor those conditions in their students, and treat them.
“I’m worried that we’re going to see long-term chronic conditions similar to what we saw with polio in the ’40s and ’50s,” said Johnson, the nurse at the University of Washington.
Johnson emphasized it’s still too early to tell whether that will happen, and what it might look like, but said nurses should be prepared.
“That role may become more prominent after — knock on wood — after we make it through this, and we begin to go back to a more normal environment in schools,” said Johnson.
Wisconsin Public Radio, © Copyright 2025, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.