In November 2020, Danielle Sigler tested approximately 200 residents in a Mount Horeb, Wis., nursing home during a COVID-19 outbreak.
The residents weren’t the only ones Sigler was worried about; 25 of her staff at Ingleside Communities also got infected.
And in the process of testing vulnerable residents, the 36-year-old nursing home administrator herself caught COVID-19. That was before the COVID-19 vaccination was available to Americans.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
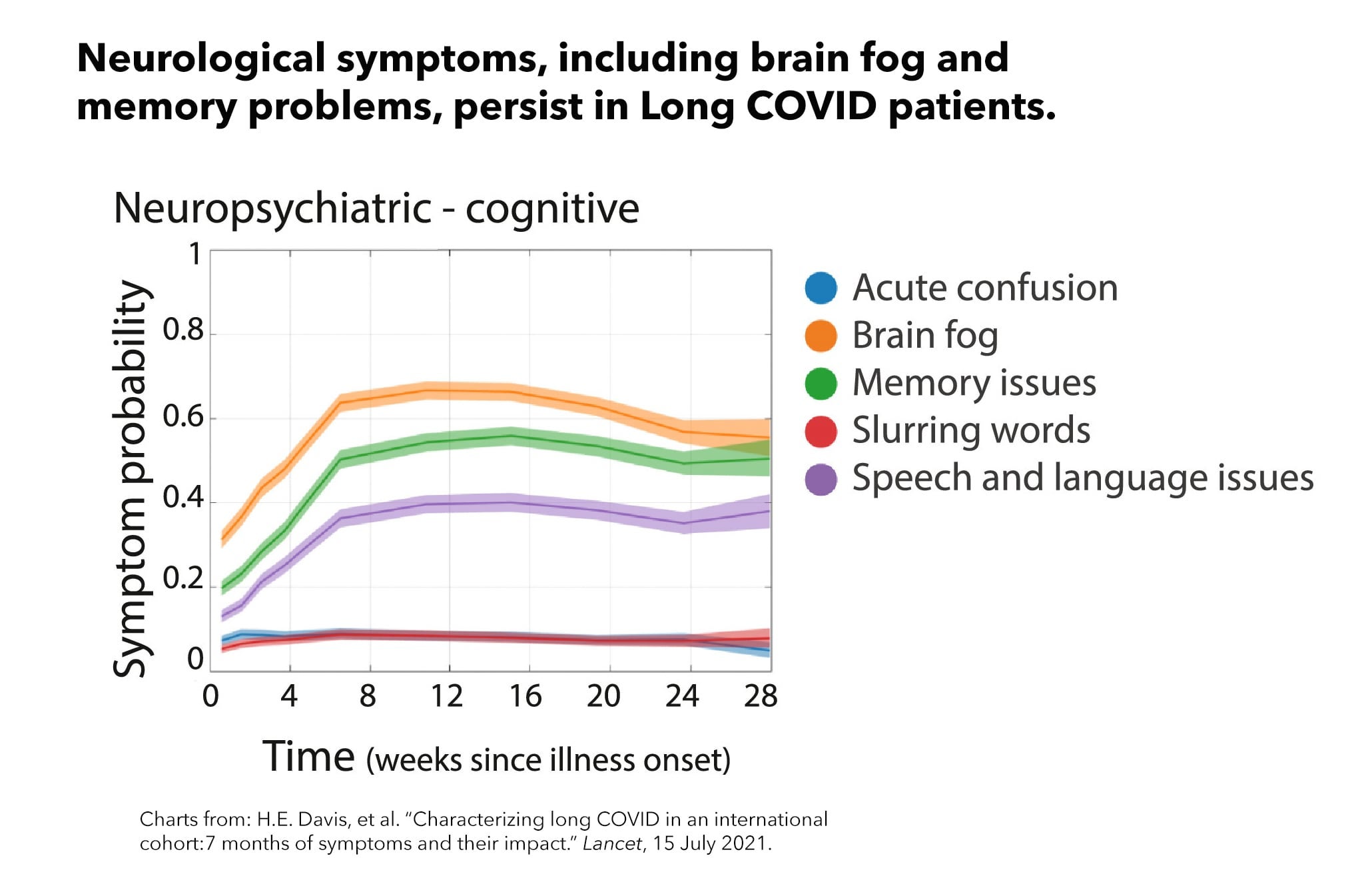
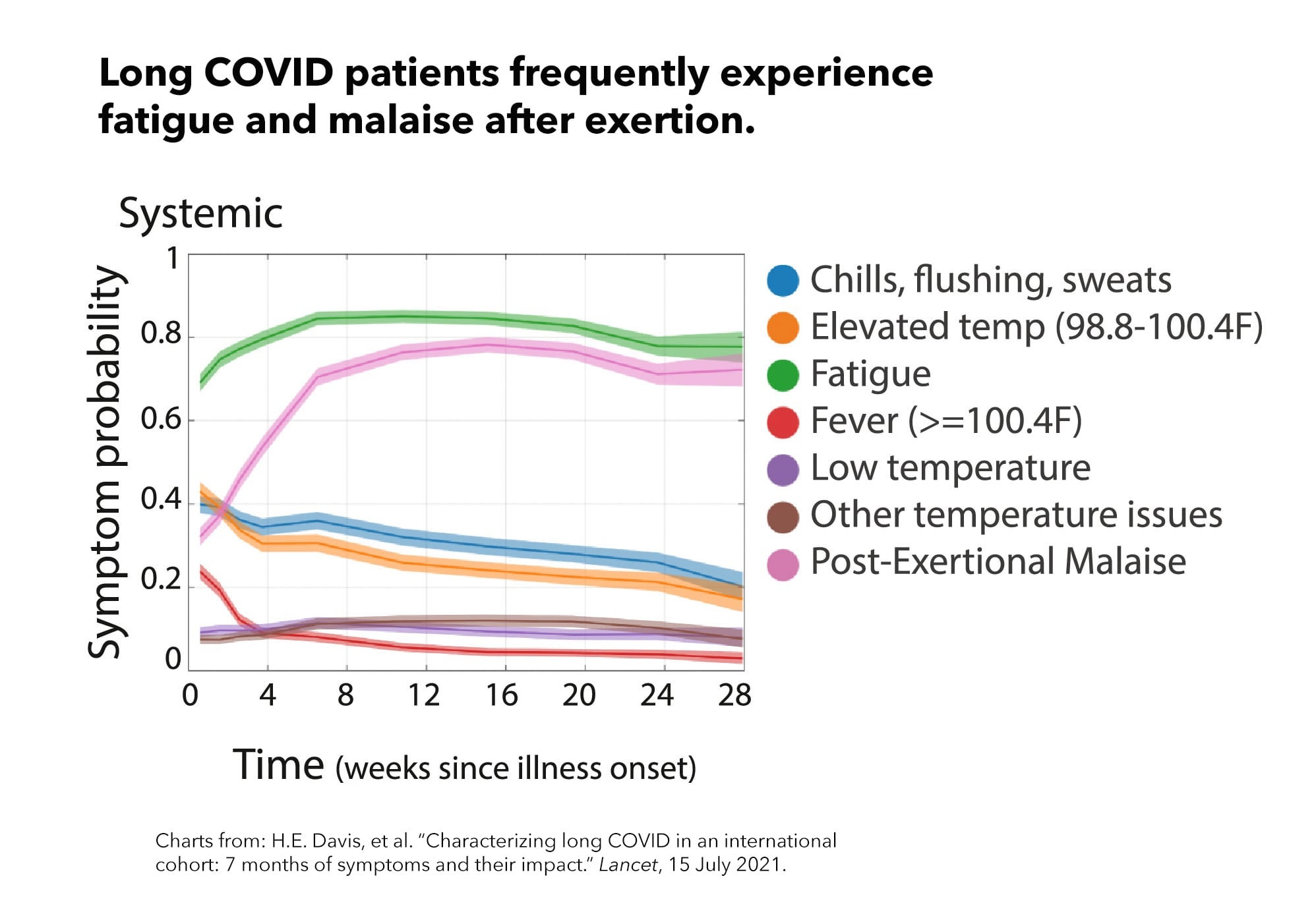
Like several of her employees, Sigler experienced so-called Long COVID, months of symptoms, including migraines, brain fog, dry cough and shortness of breath while she quarantined and worked from home.
“There were a couple of days where I just didn’t feel like I could cognitively work,” she said.
Sigler said some of her employees didn’t have paid time off or paid sick leave left, so they went to work — even when they felt bad — as a way to make ends meet. Wisconsin law does not mandate such paid benefits for employees.
Given the long-term labor shortage in the nursing home industry, Sigler said she has worked hard to keep ailing employees on the payroll through shortened shifts or changed tasks. For example, she assigned registered nurses to other duties if they could not provide direct care for residents. And she let some of her staffers take additional paid time off to keep them on the job.
“I think the government should help support them in some way or offer some sort of assistance,” Sigler said, especially for health care workers who contract COVID at work. “If they could give companies assistance with paid time off for employees, that would be helpful.”

Help for workers and their employers remains elusive. The federal government has stated that Long COVID can be considered a disability under federal law — and requires employers to provide reasonable accommodations to employees limited in their ability to work by the disease. But investigation and enforcement in such cases can take years.
As part of a set of strategies announced in early August, the federal government plans to research best practices for treating Long COVID. And it has outlined several goals to ensure that at least some of the medical costs for Long COVID are covered by Medicare, Medicaid, the Affordable Care Act and the Veterans Administration — but some of those initiatives have not yet started.
The problem is huge.
Millions of people, including more than half a million people in Wisconsin, are COVID “long haulers.” The American Academy of Physical Medicine and Rehabilitation keeps a running tally that as of Aug. 31 estimated more than 543,000 Wisconsinites had Long COVID symptoms. The U.S. Government Accountability Office estimates that 7.7 to 23 million Americans nationwide have developed Long COVID.
“Long COVID can hinder an individual’s ability to work, attend school, participate in community life, and engage in everyday activities,” said Department of Health and Human Services Secretary Xavier Becerra, whose agency leads and coordinates 13 other federal agencies in response to Long COVID.
Long COVID refers to hundreds of possible symptoms, including chronic fatigue, muscle and joint pain, shortness of breath and cognitive impairment. New data from the U.S. Census Bureau show that more than 40% of adults in the United States report having been infected, and nearly 20% of infected adults report having Long COVID symptoms.
The lingering effects can last for weeks, months or even years. Women, bisexual and transgender adults as well as Hispanic adults disproportionately are most at risk, although every demographic is affected.
The workplace impact of Long COVID
Some experts estimate 2 to 4 million U.S. employees are out of the workforce because of long-term effects of COVID-19.
“To get a sense of the sheer magnitude of that number, (4 million) is about 2.4% of the U.S. employed,” Katie Bach, who studies the role of Long COVID in the labor market shortage for the Brookings Institution, said at a congressional hearing in July.
About 44% of patients with Long COVID reported not being able to work at all, compared to their pre-COVID-19 work capacity, and 51% had reduced their working hours, according to a survey by a patients-led nonprofit COVID-19 Longhauler Advocacy Project.
Other research shows different, but still significant impacts. Preliminary evidence from KFF finds that 25% of people with Long COVID left work after infection, and 31% reduced hours, suggesting the effect on labor markets may be significant.
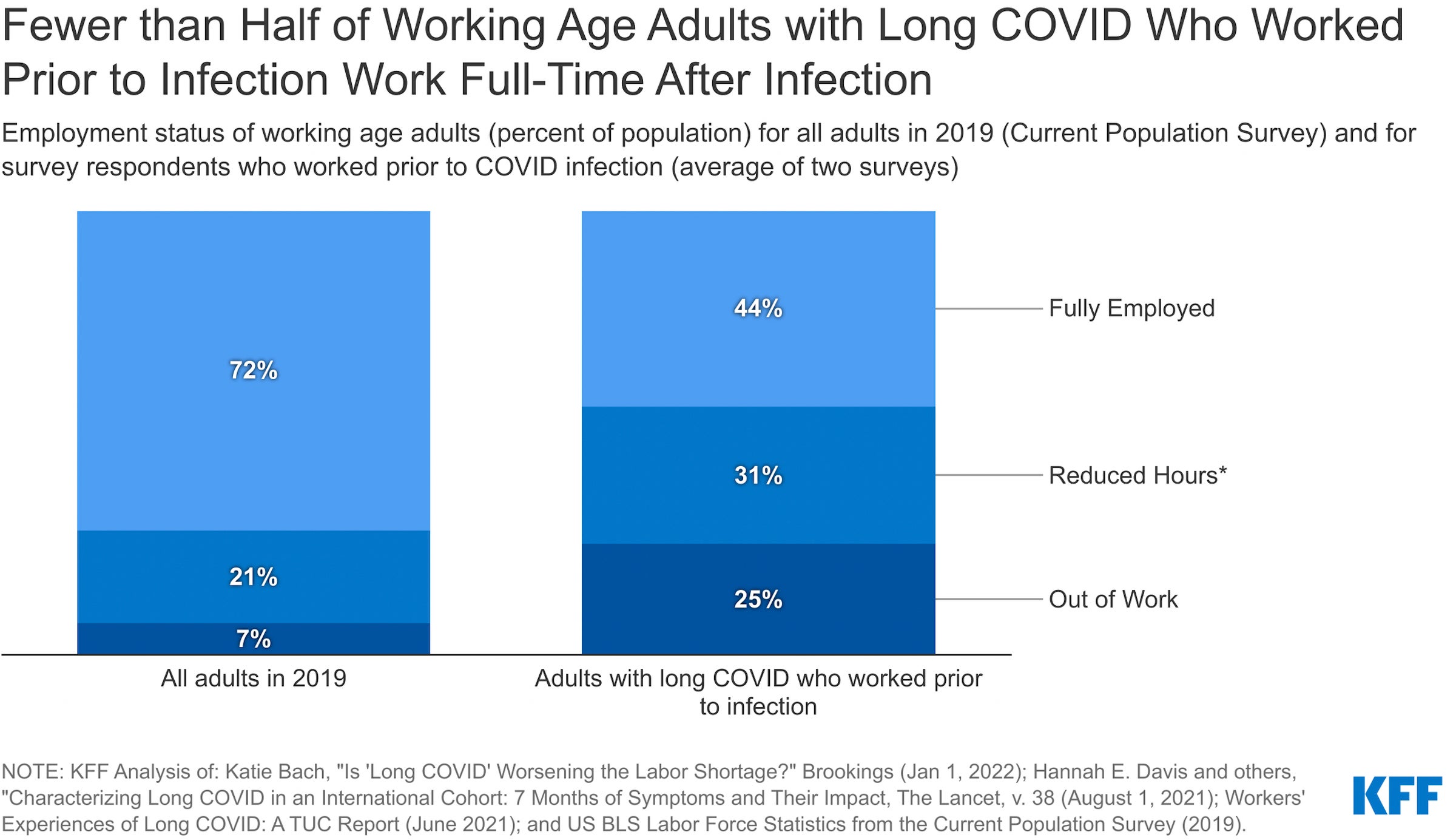
While the causes of Long COVID remain unclear, the Biden administration estimates billions of dollars in lost income and other negative effects.
“As individuals experiencing Long COVID disproportionately work in the service sector, this has led to a labor shortage in this industry, which may contribute to inflation,” according to one federal report.
A Lancet study found that cognitive dysfunction is one of the top three most debilitating symptoms that long haulers experience after six months, alongside fatigue and post-exertional malaise, the worsening of symptoms after engaging in a little bit of physical or mental activity.
Speaking at a congressional hearing in July, Hannah Davis, a coauthor of the Lancet paper and a COVID long hauler, said without further action from the lawmakers, “Long COVID will destroy our economy and disable a huge percentage of our society.”
Wisconsin workers sidelined
Among those sidelined is Georgia Linders of Onalaska After struggling for months in 2021 with debilitating symptoms typical of Long COVID, Linders was fired.
Linders began working remotely even before the pandemic for Logistics Health Inc. (LHI), a La Crosse-based military health service contractor where she had worked for almost 10 years. The former administrative assistant managed clinic contracts, making multiple phone calls daily.

Linders started experiencing low fever, sore throat, migraine and fatigue in March 2020, at the start of the pandemic when few but the most seriously ill could even be tested for COVID-19.
“I don’t have to get up, shower and drive to work,” she said. “But then if I’m still struggling to do (work) from home, then something was really, really wrong.”
Linders said her brain was slow, and answering phone calls drained her energy. She regularly updated her supervisor on her health conditions; she was told to do her best.
Linders said she was allowed to use accrued paid-time-off leave that she had earned during her career at LHI.
The accommodation didn’t last long, she said. The management team changed, and a new supervisor disciplined her.
“Georgia (Linders) is not meeting performance expectations. Specifically, she is failing to complete her work as assigned,” the new supervisor said in a document shared with Wisconsin Watch. “She is not adhering to direction provided by her leadership.”
The medical notes showed Linders felt better over the summer of 2020, but fatigue, joint stiffness and brain fog recurred in the fall. Her supervisor told her she was doing less than 30% of others’ workloads, which she said added to the stress.

She told her supervisor that her health conditions affected her work performance but was warned to expect another written warning. Around the same time, Linders was diagnosed with chronic fatigue syndrome and suspected “COVID long-haul syndrome.” She took a medical leave in November 2020 and then was on short-term disability.
In a letter shared with Wisconsin Watch, the lawyer representing LHI said the administrative termination being issued in May 2021 was made because Linders had been on leave for over six months with “no foreseeable return-to-work date.”
Long COVID as a disability
Linders filed a complaint to the Wisconsin Department of Workforce Development (DWD), claiming discrimination based on Long COVID as a disability, in August 2021. The charge is also automatically filed with the Equal Employment Opportunity Commission (EEOC), the federal fair employment enforcement agency.
Although the Biden administration has said Long COVID may be considered a disability, Linders questioned what impact that will have “unless someone is holding employers accountable when they discriminate against employees.”
Monica Murphy, managing attorney with Disability Rights Wisconsin, welcomed the federal government’s recognition of Long COVID’s long-lasting impacts on people.
“It makes clear that (Long COVID) may well fit within the disability protection,” Murphy said. According to federal guidance, Long COVID may be considered a disability “if the individual’s condition or any of its symptoms is a physical or mental impairment that substantially limits one or more major life activities.”
If Long COVID becomes disabling, employers are obligated to work with employees to come up with reasonable accommodations, such as modified work schedules, telework or reassignment to another position, according to the federal guidance. Murphy said such accommodations are often free or cost less than $500.
“Most of the many accommodations don’t have any costs to (employers),” Murphy said. “It’s just changing the way you do it or the timing of when you do something or … buying some pieces of equipment or modifying something.”
Disability Rights Wisconsin is one of the federally designated agencies across the country to provide legal assistance for long haulers. Murphy said she has given people legal advice on how to seek accommodations from employers such as telework.
Barriers to pursuing rights under the ADA
But some legal scholars argue the ADA is ineffective in protecting people with Long COVID from discrimination. The anti-discrimination law uses subjective terms of “reasonable accommodation” and “undue hardship” that can become “loopholes,” noted Angelica Guevara, an assistant professor at Indiana University-Bloomington who studies disability rights law.
Because of those provisions, if Long COVID “is starting to affect your essential functions of the job,” Guevara said, “the employer doesn’t have to keep you. He or (she) can legally let you go.”
Guevara also found the law provides limited protection for people with Lyme disease and Chronic Fatigue Syndrome, which, like Long COVID, have fatigue as a primary symptom. She added that people with these types of invisible disabilities sometimes are not believed.
And ADA cases are hard to win. Data from the federal EEOC showed that between 2011 and 2021, 64% of charges were dismissed; 21% were resolved in favor of claimants by settlement or other arrangement and just under 3% resulted in a finding of discrimination.
In Linder’s case, after months of investigation, EEOC dismissed her complaint, making no determination on discrimination and advising that she may bring a court action. She decided to drop the matter, citing expense and unlikelihood of proving she’d been discriminated against.
In a letter shared with Wisconsin Watch, the lawyer representing LHI said Linders cannot claim Long COVID as a disability since she had never been diagnosed with the infection.
Linders took her first COVID-19 test one month after her initial symptoms and then tested another time. Both results showed negative. Some long haulers report testing negative but still experiencing Long COVID symptoms.
The U.S. Department of Labor has urged employers to provide accommodations even for employees who don’t get an official Long COVID diagnosis.
“Your focus should be on the employee’s limitations and whether there are effective accommodations that would enable the employee to perform essential job functions,” the labor agency said in its guide for employers on how to support workers with Long COVID.
Some Wisconsin employers accommodate
Like Sigler, Bach told Wisconsin Watch that many employers may be motivated to provide accommodations to help people remain productive because hiring and training new employees in a tight labor market can be difficult and expensive.
Wisconsin’s nursing home industry in particular is facing a labor shortage crisis. Despite offering competitive packages, including tuition reimbursement, Sigler said she has advertised jobs that get just one applicant.
And even though many employers have shifted to remote or hybrid work models, some cannot provide flexible options. Sigler said her business requires most staff to physically be at work.
But from personal experience, she knows how debilitating Long COVID can be.

Sigler returned to work on day 11 after being infected when some other staffers were quarantined at home for two to three weeks. Sigler worked 12-hour night shifts while struggling with a 103-degree fever, insomnia, sweats, and disorientation.
“It was a really weird euphoric feeling at the end of the day,” she said.
She said her intensive workloads slowed her recovery, and her body was “destroyed.”
Alexia Kulwiec, an associate professor at the University of Wisconsin-Madison’s School for Workers, said she would like to see the federal government return to providing tax incentives for employers who provide paid sick leave for people with Long COVID.
Under the Families First Coronavirus Response Act, employers providing paid leave for up to two weeks to employees for COVID-19 could receive reimbursements in the form of tax credits, but the program ended in March 2021.
“It’s very disheartening to see that the policies that came out during COVID have essentially been reversed and undone, so they’re not there to protect employees today,” Kulwiec said.
A ‘mass disabling event;’ stalled federal supports
The federal government plans to establish a Long COVID office within the Department of Health and Human Services overseeing research and coordinating activities between federal agencies, patients, researchers and physicians. But how and when it will be funded and staffed remains unclear.
“Nothing can be done until they get funded. You would think the number of workers affected by this illness would encourage them to get funding,” Linders said, noting that Long COVID has been dubbed a “mass disabling event.”
Linders is now receiving Social Security Disability benefits — the last resort for many COVID long haulers.
“It is a difficult and a lengthy process,” said Eva Shiffrin, a managing Attorney at Disability Rights Wisconsin. “Anything that can be done in general to shorten the lengthy process, including eliminating the five-month wait period, would help all Social Security Disability seekers including those with Long COVID.”
Back in Dane County, Sigler is still experiencing fatigue, migraines and gastrointestinal issues, and some of her staffers also still struggle with Long COVID.
“If anything, we’ve learned and worked with the pandemic,” she said. “We’ve learned to be creative. We’ve learned to work with what we have, and people have skills we can still utilize. So how best to utilize them and still maintain their health?”
The nonprofit Wisconsin Watch (www.WisconsinWatch.org) collaborates with WPR, PBS Wisconsin, other news media and the University of Wisconsin-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by Wisconsin Watch do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.







